In 2025, the global ambulatory surgery centres (ASCs) IT services market is expected to hit $10.13 billion, driven by the growing demand for accurate, efficient, and compliant billing processes. As reimbursement complexities continue to grow, ASCs face various challenges from solving evolving coding standards to reducing claim denials and ensuring steady cash flows.
An Ambulatory Surgery Center (ASC) specializes in outpatient procedures, including surgeries, pain management, and diagnostic treatments like colonoscopies. These procedures are more complex than those in a typical doctor’s office, but don’t require a hospital stay. In this blog, we will explore why it is important to bill accurately and efficiently for ASC.
Why Precise ASC Billing and Coding Matters?
Managing billing and coding for an ambulatory surgery centre is crucial. It not only includes submitting claims but also involves managing compliance, understanding payers’ specific requirements, and ensuring every procedure is performed timely and accurately. The complexity is compounded by frequent changes to CPT and HCPCS codes, updates to ASC Payment Systems, and the need to manage both physician and facility billing. Missing even a small detail can cause significant revenue leakage.
Common Challenges in ASC Billing and Coding
Despite the advancements, ASCs face several challenges in their billing and coding operations:
Complex Regulatory Environment:
The Centers for Medicare & Medicaid Services (CMS) frequently updates payment policies, necessitating ASCs to stay abreast of changes to avoid compliance issues. For instance, the January 2025 ASC payment system update introduced new device categories and billing instructions, impacting reimbursement structures.
Disparities in Procedure Costs:
Recent studies have highlighted significant cost variations for similar procedures performed in different settings. In New York, the average cost for routine, low-complexity medical procedures is four times higher at outpatient hospital facilities compared to doctors’ offices, primarily due to additional facility fees. Such disparities can complicate billing processes and affect patient satisfaction.
Outsourcing Medical:
Outsourcing medical billing services can free up your hands and prevent you from investing in costly options like hiring an in-house team. And then providing them with the training can be very challenging. While these solutions offer numerous benefits, integrating new systems with existing workflows can be challenging.
Using Advanced Solutions
To address these challenges, ASCs are increasingly turning to sophisticated IT services designed to improve the billing and coding processes. Key solutions include:
- Electronic Health Records (EHRs): Implementing EHRs can reduce human errors and increase overall operational efficiency by improving administrative activities, patient data management, scheduling, billing, and inventory management.
- Cloud-Based Solutions: Adopting cloud-based platforms like Health Quest allows for scalable and flexible management of billing and coding operations, facilitating real-time updates and remote accessibility.
Covered Services Under ASC Reimbursement
When filing ASC claims, it’s crucial to note that the services eligible for reimbursement vary depending on the specific type of facility. The ASC facility’s status directly influences the coverage under ASC guidelines.
While certain services are generally considered outside the scope of typical ASC services, they may still be reimbursed if provided by an ASC. These include:
- Non-Implantable Durable Medical Equipment
- Leg, Arm, Back, and Neck Braces
- Physician Services
- Prosthetic Devices
- Independent Laboratory Services
- Ambulance Services
- Artificial Limbs (Legs, Arms, Eyes)
- Implantable Durable Medical Equipment
Key CMS Updates Impacting ASC Billing in 2026
To stay ahead of reimbursement changes, ASCs need to prepare for the proposed 2026 CMS updates to the Ambulatory Surgical Center Payment System. These updates highlight both new opportunities and challenges for outpatient facilities.
Key Highlights for 2026:
- 2.4% Reimbursement Increase: ASCs that meet quality reporting requirements will see a 2.4% payment adjustment. This is slightly lower than the 2.9% update in 2025, reflecting a 3.2% hospital market basket increase offset by a 0.8% productivity adjustment.
- Hospital Market Basket Updates Extended: CMS will continue using the hospital market basket methodology through 2026 while monitoring ASC utilization and costs.
- New Payment Indicator – “S2”: Skin substitute products provided with covered ASC procedures will now be separately payable at OPPS rates, rather than bundled.
- Expansion of Covered Procedure List (CPL): CMS has proposed changes to ASC exclusion criteria, potentially allowing more procedures to qualify for ASC reimbursement.
- Speciality Payment Impacts:
- Cardiovascular procedures: +12%
- Genitourinary procedures: +18%
- Eye surgeries: –2%
- Other categories (musculoskeletal, digestive) may see moderate increases (1–3%).
- Cardiovascular procedures: +12%
Strategies for Improving Billing and Coding Of ASCs
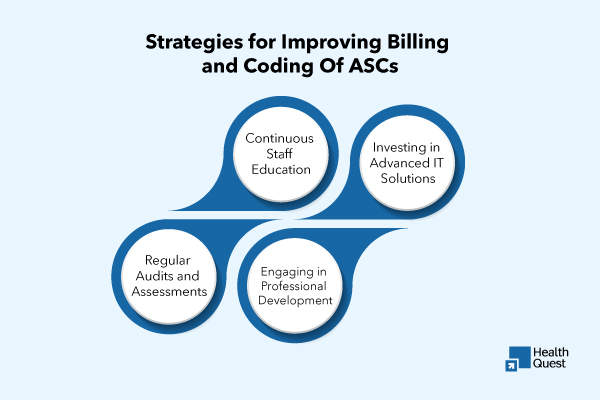
To grow in the evolving landscape, ASCs should consider the following strategies:
- Continuous Staff Education: Regular training ensures that billing and coding staff are updated on the latest codes, regulations, and best practices, reducing the risk of errors.
- Investing in Advanced IT Solutions: Allocating resources towards modern IT infrastructure, such as AI-driven documentation tools and comprehensive EHR systems, can enhance efficiency and accuracy.
- Regular Audits and Assessments: Conducting periodic audits helps identify areas of improvement, ensuring that billing and coding processes align with current standards and regulations.
- Engaging in Professional Development: Participating in specialized courses, such as the “Coding & Reimbursement for ASCs” virtual course, provides essential training and insights from industry experts, equipping staff with strategies to maximize reimbursements.
Also read: Ambulatory Surgery Center (ASC) Billing Strategy 2025
Key Compliance Factors in ASC Billing
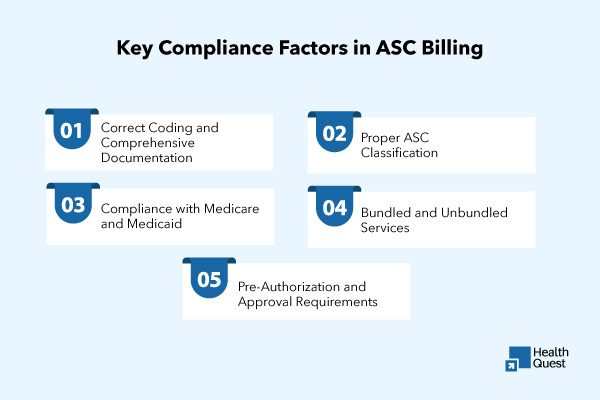
When it comes to billing in Ambulatory Surgery Centers (ASCs), maintaining compliance is critical. Ensuring accurate reimbursement while avoiding legal and financial risks depends on following strict guidelines. Here are the essential compliance factors to consider in ASC billing:
Correct Coding and Comprehensive Documentation
- ICD-10-CM Diagnosis Codes: Ensure all diagnosis codes accurately represent the patient’s condition. Any mistake or omission in these codes could lead to claim denials or an increased risk of audits.
- CPT Procedure Codes: It’s vital to use the right CPT codes that match the procedures performed. Incorrect coding can result in claim disputes, underpayments, or audits.
- Modifiers: Applying the correct modifiers (such as modifier 22 for unusual services or modifier 59 for distinct procedural services) clarifies special circumstances in the provided procedure, helping prevent payment issues.
Proper ASC Classification
- Billing under the Right Category: Confirm that services provided are billed under the correct ASC classification. ASCs have distinct billing requirements, separate from hospital outpatient or physician office services. Ensure your ASC meets CMS guidelines to qualify for the appropriate reimbursement.
Compliance with Medicare and Medicaid
- Medicare Coverage: Ambulatory Surgery Centers must comply with specific Medicare rules, including the types of services covered and the associated reimbursement policies. It’s crucial to stay updated on regional variations in Medicare coverage for ASCs.
- State-Specific Medicaid Rules: Medicaid regulations can differ from state to state. Make sure you understand and adhere to your state’s particular Medicaid billing guidelines, including covered services and allowable rates.
Bundled and Unbundled Services
Many ASC procedures come with bundled payments, meaning several related services are paid under one code. Billing separately for services included in a bundle (unbundling) can result in penalties. Understanding which services can be bundled and which must be billed separately is essential to avoiding overpayments or underpayments.
Pre-Authorization and Approval Requirements
Certain insurers, particularly Medicare Advantage plans, may require pre-authorization before certain procedures are performed. It’s crucial to obtain all necessary pre-approvals in advance and ensure they are properly documented, as failing to do so could lead to claim denials.
CPT Codes for ASCs
|
Category |
CPT Codes |
|
Surgical Procedures |
10021-69990 (Various CPT codes for surgery) |
|
Diagnostic Services |
36415 (Blood draw), 93000 (ECG) |
|
Anesthesia |
00100-01999 (Anesthesia services) |
|
Laboratory Tests |
80047-89398 (Various lab tests) |
|
Durable Medical Equipment |
99070 (Supplies used in surgery), 99299 (Unlisted codes) |
|
Therapy Services |
97110-97799 (Therapy services) |
|
Postoperative Care |
99024 (Postoperative care visits) |
|
Pain Management |
64400-64999 (Pain management injections) |
ICD Codes for ASCs
|
Category |
ICD Codes |
|
Surgical Procedures |
ICD-10 codes for specific diagnoses and procedures |
|
Diagnostic Services |
ICD-10 codes for diagnostic purposes (e.g., Z00.00 for general exams) |
|
Anesthesia |
ICD-10 codes for anaesthesia-related conditions (e.g., R40.0 for coma) |
|
Laboratory Tests |
ICD-10 codes for conditions leading to testing (e.g., E11 for Type 2 diabetes) |
|
Durable Medical Equipment |
ICD-10 codes for related conditions (e.g., Z96.1 for prosthetic joint) |
|
Therapy Services |
ICD-10 codes related to therapy conditions (e.g., M54.5 for low back pain) |
|
Postoperative Care |
ICD-10 codes related to recovery or complications (e.g., T81.4 for post-surgical infection) |
|
Pain Management |
ICD-10 codes for pain-related conditions (e.g., G43 for migraines) |
Final Thought:
Dealing with the complexities of ambulatory surgery centres’ billing and coding requires a multifaceted approach that includes staying informed about regulatory changes, investing in advanced technologies, and fostering continuous education. By implementing these strategies, ASCs can enhance their operational efficiency, ensure compliance, and optimize their revenue cycles in an ever-evolving healthcare landscape.
Schedule an appointment with Health Quest Billing today at (415) 508-6537 to streamline your ASC billing and coding.