Medicaid provides healthcare coverage to more than 70 million people – about one in five Americans. For providers, learning how to bill Medicaid can feel overwhelming at first, but with the right steps, it becomes a manageable process. Mastering Medicaid billing ensures you get paid for your services while continuing to deliver quality care to patients who need it most.
What Is Medicaid?
Medicaid is a joint federal and state program that provides health care coverage to low-income individuals, including children, pregnant women, the elderly, and people with disabilities. It ensures access to medical services for those who cannot afford private insurance.
Medicare & Medicaid Billing
The Medicare and Medicaid billing process is how providers submit claims to get reimbursed for patient care. It’s highly regulated and can be complex, since each program has its own rules. Medicare rates are set federally, while Medicaid rates vary by state. Understanding both helps providers receive accurate payments and ensures patients continue getting needed care.
Agencies in behavioral health, mental health, and substance abuse may find billing especially challenging, but following CMS guidelines and streamlining workflows keeps claims accurate, payments timely, and care uninterrupted.
Who are medicaid providers?

Medicaid providers include a variety of healthcare professionals and organizations that deliver medical services to Medicaid recipients. Here’s a list of common Medicaid providers:
- Doctors
- Hospitals
- Nursing Homes
- Pharmacies
- Dentists
- Mental Health Providers
- Home Health Agencies
- Laboratories
- Durable Medical Equipment Suppliers
Read: How to Bill Medicare
Medicare Coverage & Billing Guidelines
Medicare billing rules vary depending on whether you’re billing for Part A, B, C, or D services. To avoid denials and ensure faster reimbursements, providers must always verify coverage through the Medicare Coverage Database or the patient’s Medicare Administrative Contractor (MAC). Each part has its own requirements, from inpatient hospital billing under Part A to prescription drug claims under Part D.
| Part | Coverage | Billing Guidelines |
|---|---|---|
| A | Inpatient hospital, skilled nursing, hospice | Include Medicare number, admission date, and diagnosis codes. Confirm services are medically necessary. |
| B | Outpatient care, doctor visits, lab tests, equipment | Verify medical necessity and confirm coverage before billing. |
| C | Medicare Advantage (private plans covering A & B) | Bill directly to the plan using its instructions. Each plan may have unique rules – check before submitting. |
| D | Prescription drugs | Submit claims to the drug plan as instructed. Physician’s written order required. Remind patients about the coverage gap. |
How to Bill Medicaid as a Healthcare Provider
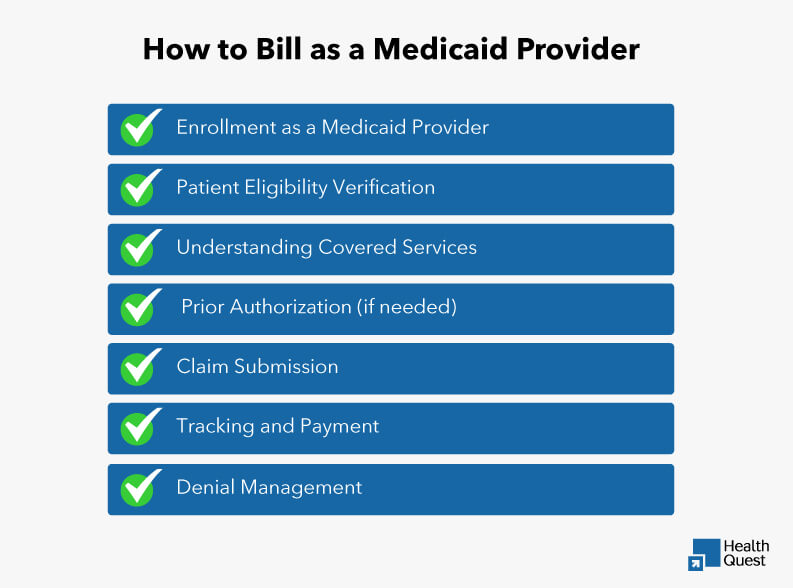
Billing Medicaid as a provider can seem like a complex process, but understanding the key steps and requirements can make it much more manageable. It’s important to ensure that you are properly enrolled, verify patient eligibility, understand the services covered by Medicaid, and follow the correct procedures for claim submission and payment tracking. Here’s a breakdown of the steps involved:
Enrollment as a Medicaid Provider
Before you can bill Medicaid, you need to enroll as a provider with your state’s Medicaid agency. This step is crucial because it ensures that you are recognized and authorized to submit claims for services provided to Medicaid recipients. Medicaid enrollment is the foundation of your ability to receive reimbursement for services rendered.
- Registration: Register through your state’s official portal.
- NPI: Obtain a National Provider Identifier (NPI).
- State-Specific: Enrollment procedures vary by state, so make sure to follow your state’s specific guidelines.
Patient Eligibility Verification
Before each patient visit, it’s essential to verify their Medicaid eligibility. This step ensures that the patient is covered for the services you are providing and helps prevent claim denials or delays due to eligibility issues. Medicaid eligibility can change frequently, so verifying it before each visit ensures you’re providing care to eligible patients and that you can be reimbursed for your services.
- Verify Coverage: Check patient eligibility before each visit via the state’s portal or your EHR system.
- Check Plan Type: Confirm the Medicaid plan and any limits or third-party insurance.
Understanding Covered Services
Medicaid provides healthcare coverage, but it only covers specific services, which can vary by state. It’s essential for healthcare providers to fully understand the services covered under Medicaid, the reimbursement rates, and any prior authorization requirements in order to avoid claim denials and ensure timely payments.
- Fee Schedule: Review your state’s Medicaid fee schedule for covered services and reimbursement rates.
- Prior Authorization: Some services require prior authorization. Be sure to gather the necessary documentation to support the request.
- Exclusions: Check for any service exclusions specific to your state’s Medicaid program.
Prior Authorization (if needed)
Some Medicaid services require prior authorization before they can be billed to Medicaid. This process ensures that the services are medically necessary and covered under the patient’s Medicaid plan. Without prior authorization, claims may be denied, resulting in delayed payments and potential financial setbacks for the provider. Here’s a closer look at the prior authorization process:
- Documentation: For services requiring prior approval, submit the necessary documents (e.g., CPT/ICD codes, medical necessity).
- Tracking: Follow up on authorization requests until approval or denial.
Claim Submission
Once you’ve provided services to your Medicaid patients, the next step is submitting the claims. Accurate and timely claim submissions are crucial for receiving payment. A well-submitted claim helps reduce the risk of denials and ensures the practice is reimbursed for the services rendered. Here’s a breakdown of how to submit claims correctly:
- Claim Forms: Use the appropriate claim forms (CMS-1500 for professional services, UB-04 for institutional services).
- Accurate Information: Include all necessary details such as patient and provider information, service codes, and place of service.
- Submission Methods: Submit claims electronically through your EHR system, clearinghouse, or state portal.
Tracking and Payment
Once you’ve submitted your Medicaid claim, the next critical step is to track its status and ensure payment is received. Monitoring your claims helps identify any issues early and ensures you’re paid for the services provided. Here’s how to effectively track your claims and manage the payment process:
- Claim Status: Monitor claim status through the Medicaid portal or clearinghouse.
- Remittance Advice: Check remittance advice for payment details and any denials or underpayments.
- Payment Matching: Match received payments to submitted claims.
Denial Management
It’s essential to know how to handle denied Medicaid claims effectively. Understanding why a claim was denied, identifying the errors, and addressing them quickly can help ensure that you’re reimbursed for the services you provide. By tackling denials head-on, you can reduce delays and keep your practice’s cash flow steady.
- Denial Codes: Understand the reason for any denied claims by reviewing denial codes.
- Correct and Resubmit: Fix any identified errors and resubmit the claim within the timely filing deadline.
Appeals Process for Denied Claims
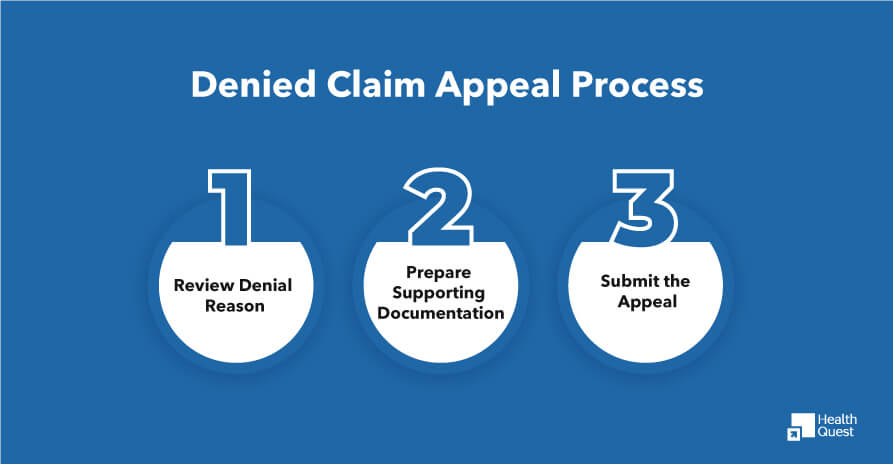
When Medicaid claims are denied after resubmission, it’s essential to know how to appeal the decision. The appeals process ensures you have the opportunity to correct any errors and provide additional information to support your claim. Here’s a quick guide on how to initiate an appeal:
Review Denial Reason:
First, carefully review the denial code and reason provided by Medicaid. This will help you understand why the claim was rejected. If the denial is due to coding errors, missing documentation, or medical necessity issues, these must be addressed in the appeal.
Prepare Supporting Documentation:
Collect all relevant documents to support your case. This may include updated medical records, detailed physician notes, or test results that justify the service provided.
Submit the Appeal:
Follow your state’s Medicaid guidelines for submitting appeals, making sure to meet deadlines. Submit the appeal with clear, concise language explaining the error and why the claim should be reconsidered.
Types of Denial Appeals:
- First-Level Appeals: This is the initial stage of the appeal process. If a claim is denied, you can submit a first-level appeal where you provide additional documentation or clarification to correct the denial. Common reasons for first-level appeals include missing codes, incorrect service dates, or failure to meet Medicaid’s medical necessity criteria.
- Second-Level Appeals: If the first-level appeal is unsuccessful, a second-level appeal can be initiated. This stage often requires a more detailed review and may involve a formal hearing or submission of additional supporting evidence. Second-level appeals are typically used for complex cases where the issue isn’t resolved at the first stage.
Tips for a Strong Appeal:
Using these tips can help you appeal your claims efficiently.
Highlight Medical Necessity: If the denial is related to medical necessity, provide clear evidence that the treatment or service was essential for the patient’s health.
Correct Coding Errors: If the claim was denied due to incorrect coding, ensure the codes are updated to reflect the accurate diagnosis and procedures. Use proper CPT, ICD, or HCPCS codes to avoid further issues.
Revalidation of Provider Enrollment
Medicaid providers must periodically go through a revalidation process to maintain their enrollment status. This process typically occurs every 5 years, but can vary by state. During revalidation, providers need to verify their information and ensure compliance with Medicaid requirements.
Why should you, as a provider, treat Medicaid Patients?
There are several reasons you should treat medicaid patients. As a healthcare provider, you are ethically obliged to treat all kinds of patients, regardless of what their healthcare insurance is. Here are some benefits of treating medicaid patients.
Ethical Obligations:
You, as a healthcare provider, are obligated to provide services to every patient who visits you, and that is your professional and social responsibility. This can increase the trust between a patient and a healthcare provider.
Clinical and Public Health Advantages
Access to healthcare can help in managing chronic conditions. This can also build a trust relationship between the deserving people and the healthcare providers.
Increased revenue:
In the US, every 1 in 5 people has a medicaid insurance plan, which makes it more beneficial for you. It can boost your revenue. More patients mean more revenue, which can lead to financial stability.
Final Thought:
Billing Medicaid as a provider may seem overwhelming at first, but with the right knowledge and tools, it becomes a manageable and rewarding process. Understanding Medicaid enrollment, eligibility verification, covered services, and the appeals process is essential to ensuring that you are reimbursed for the services you provide. By following these steps and staying compliant with state-specific rules, you can reduce denials, speed up payments, and focus on what matters most: providing quality care to your patients.