Hospitals across the U.S. are facing a growing crisis: they’re losing money on nearly every Medicare patient they treat. According to a 2025 report by the AAMC, American hospitals collectively lost $4.9 billion on Medicare hospitalizations in 2021, averaging a $2,244 loss per inpatient discharge. For not-for-profit teaching hospitals, that figure soared to over $5,800 lost per complex Medicare case.
While hospitals can’t control the reimbursement rates set by Medicare, they can control how accurately and efficiently they bill for services. That’s where partnering with an experienced medical billing company becomes a game-changer.
In this article, we’ll break down:
-
Why hospitals lose money on Medicare patients
-
How professional billing services can help mitigate those losses
-
Specialty-specific billing strategies for high-risk departments
-
A breakdown of Medicare’s payment models and how to navigate them
-
The long-term financial impact of underpayments—and how to fight back
Why Are Hospitals Losing Money on Medicare?
According to the AAMC report and other national analyses, the financial strain stems from a combination of structural underpayments and preventable billing inefficiencies. Here’s what’s contributing to the problem:
Only 3.9% of DRGs are profitable
Most Diagnosis-Related Groups (DRGs) under Medicare fail to provide sufficient reimbursement to cover the cost of care.
CMS Sets Low Reimbursement Rates
Medicare’s fixed rates are often below actual service costs, particularly in high-acuity, high-complexity cases like ICU care, surgical recovery, and rehabilitation.
Documentation & Coding Errors
Incorrect or incomplete documentation leads to lower-paying DRG assignments, underpayments, or denials, even when the care was more complex.
The root causes include:
- Low fixed reimbursement rates from CMS
- Coding and documentation errors that lower DRG reimbursements
- High denial rates and slow appeals processes
- Poor visibility into claims performance and payment trends
How Medical Billing Experts Help Hospitals Reduce Medicare Losses

When hospitals lose money on almost every Medicare patient, it’s not just frustrating, it’s unsustainable. The good news? A skilled medical billing partner can make a big difference. Here’s how billing experts help healthcare providers recover revenue and stay ahead.
Get More Claims Paid the First Time
Every denied claim wastes time, delays cash flow, and adds to your team’s stress. Billing companies help improve your clean claim rate, which means more of your Medicare claims get paid without rework.
Here’s how they do it:
- Follow Medicare-specific billing rules to avoid rejections
- Flag issues like missing modifiers or diagnosis mismatches
- Catch errors early with claim scrubbing tools
Tackle Denials Head-On
Medicare doesn’t make it easy, especially when it comes to complex cases. But denial doesn’t have to mean dead-end. Billing specialists track trends, file smart appeals, and fight for every dollar you’ve earned.
They help by:
- Spotting denial patterns in high-cost DRGs
- Writing strong, timely appeals backed by documentation
- Recovering payments from aging A/R and secondary payers
Make Sure Your Coding Tells the Full Story
A lot of hospitals don’t realize they’re being underpaid just because their coding doesn’t reflect the full complexity of care. Billing professionals work with your documentation team to make sure nothing gets missed.
They ensure:
- Accurate DRG coding based on what was actually treated
- Better documentation with CDI (Clinical Documentation Improvement) support
- Compliance with Medicare rules to avoid audits and underpayments
Help You Get Credentialed with the Right Plans
Medicare Advantage plans often pay better than traditional Medicare. But getting set up with them takes time. Billing partners can manage the entire credentialing process so you don’t miss out on better contracts.
What they do:
- Handle eMedNY, CAQH, and MCO enrollment
- Recommend top-performing plans in your area
- Help expand your Medicare payer mix
Show You Exactly Where You’re Losing Money
Most hospitals don’t have the tools to track Medicare claims in real time. A billing partner brings data to the table so you’re not left guessing where the problems are.
You get:
- Dashboards that show clean claim rates, denial trends, and payment gaps
- Reports that highlight which DRGs are losing money
- Easy-to-understand insights for leadership teams
Keep You Compliant and Audit-Ready
Medicare billing rules change all the time and small mistakes can lead to big penalties. A billing company helps you stay compliant and audit-proof with regular checks and training.
How they help:
- Run quarterly compliance audits on Medicare claims
- Catch over coding, under coding, and risky patterns
- Keep your team updated on CMS policy changes
High-Loss Specialties’ Need Extra Support
Some specialties like behavioral health, inpatient rehab, and chronic care are hit hardest by Medicare underpayments. These services are complex, time-intensive, and often reimbursed far below cost.
A skilled billing partner can help by:
Accurate specialty-specific coding
Ensures complex conditions and services are properly captured and billed at the highest appropriate level.
Improved documentation support
Helps providers and clinical teams document time-based services, severity levels, and medical necessity key for behavioural health and rehab claims.
Targeted denial tracking and appeal strategy
Analyzes common denial reasons in specialties like mental health (e.g., medical necessity denials) and develops appeal templates that work.
Optimized billing for bundled care
Chronic care and transitional care often involve bundled Medicare billing codes; these require careful tracking and timing to be reimbursed correctly.
Support for community-based and telehealth models
Many high-risk specialties use alternative care models. A billing partner ensures compliance with Medicare’s evolving guidelines for telehealth, IOP (Intensive Outpatient Programs), and home-based services.
Medicare Payment Models Overview
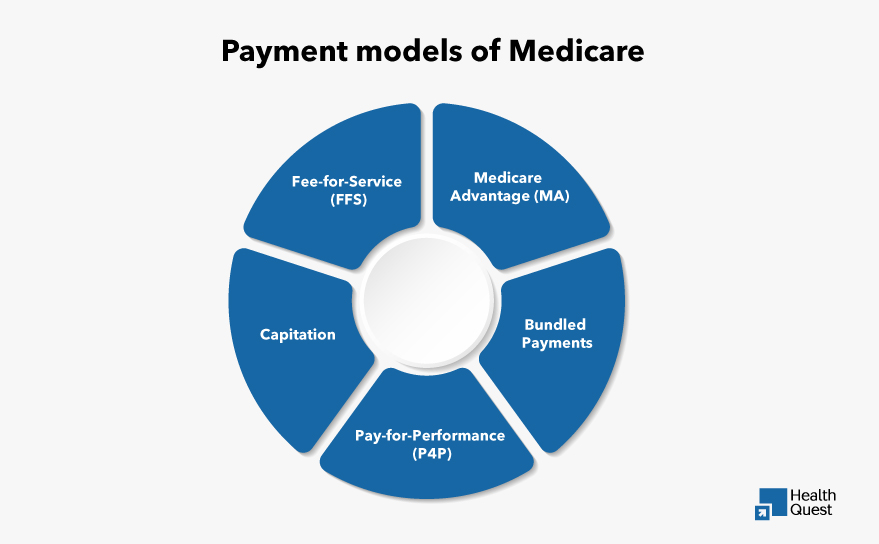
Hospitals can reduce Medicare-related losses by understanding the different Medicare payment models and optimizing their billing strategies. Here are the main models:
| Model | Overview | Optimization Tip |
|---|---|---|
| Fee-for-Service (FFS) | Paid per individual service | Ensure accurate codes and thorough documentation |
| Medicare Advantage (MA) | Managed by private insurers; may offer higher rates | Partner with high-performing plans and manage contracts |
| Capitation | Fixed monthly rate per patient | Focus on preventive care and efficient care delivery |
| Bundled Payments | One payment for related services over time | Coordinate care and use accurate time/service coding |
| Pay-for-Performance (P4P) | Payments tied to quality metrics | Improve outcomes and meet CMS quality benchmarks |
Fee-for-Service (FFS):
In this model, hospitals get reimbursed for each individual service they provide. While it offers payments for every service, the reimbursement rates are often low, underpayments can also occur. Hospitals can improve by ensuring that the codes and documents are accurate.
Medicare Advantage (MA):
Medicare contracts with private insurers to provide coverage. These plans typically offer higher reimbursement rates than traditional Medicare, but the payment can vary depending on the insurer. Hospitals should partner with high-performing plans and ensure proper contract management.
Capitation:
Hospitals receive a fixed payment per patient per month, regardless of the services provided. While this model offers predictable payments, hospitals bear the risk of costs exceeding the fixed rate. The key to optimization is efficient care delivery and proactive prevention.
Bundled Payments:
A single fixed payment is given for a group of related services provided over a specific period. While it encourages coordinated care, it also means hospitals are responsible for managing costs within the payment. Accurate coding and effective care coordination are essential.
Pay-for-Performance (P4P):
Hospitals are reimbursed based on the quality of care provided, rather than the volume of services. This model rewards high-quality care with bonuses but penalizes poor performance. Hospitals must focus on improving patient outcomes and meeting quality metrics.
Financial Impact of Underpayments
Medicare underpayments can have serious long-term consequences for hospitals, extending beyond immediate operational losses. Here’s how:
Reduced Cash Flow
Underpayments limit cash flow, making it harder for hospitals to cover operational expenses and pay staff, which can disrupt day-to-day operations.
Operational Challenges
Ongoing underpayments force hospitals to reduce or delay services, which affects patient care and hinders growth or new initiatives.
Staffing Issues
Hospitals may need to cut staff or reduce benefits to manage costs, leading to burnout, increased turnover, and ultimately, lower quality of care.
Limited Access to Technology
Underpayments prevent hospitals from investing in essential medical technologies, limiting their ability to provide high-quality care and stay competitive.
Long-Term Financial Health
If underpayments persist, hospitals risk long-term financial instability, which could lead to service reductions, mergers, or even closures.
Final Thoughts:
Partnering with an expert medical billing company like Health Quest can make all the difference in managing your hospital’s Medicare billing, improving reimbursement rates, and reducing costly underpayments.
Contact us today to learn how our billing experts can optimize your claims, tackle denials, ensure coding accuracy, and provide actionable insights to boost your bottom line. Let’s work together to secure your hospital’s financial health and long-term sustainability!