As 2026 approaches, healthcare providers across the United States will face significant changes to the Centers for Medicare & Medicaid Services (CMS) regulations. These updates will affect Medicare Fee-for-Service, Medicare Advantage, Medicaid, CHIP, and delegated credentialing systems. The stakes are higher than ever, and the margin for error is shrinking.
Failure to comply with CMS’s updated requirements could lead to costly fines, service disruptions, and operational inefficiencies. For healthcare providers, these changes call for a shift from a “best-effort” compliance strategy to a more structured, auditable, and proactive process that ensures timely and accurate data management across all systems.
With these changes rapidly approaching, it’s crucial for healthcare organizations to take immediate steps to prepare. In this blog, we explore the critical CMS changes for 2026 and how providers can navigate these challenges to ensure compliance and mitigate risks.
Key CMS Changes for 2026
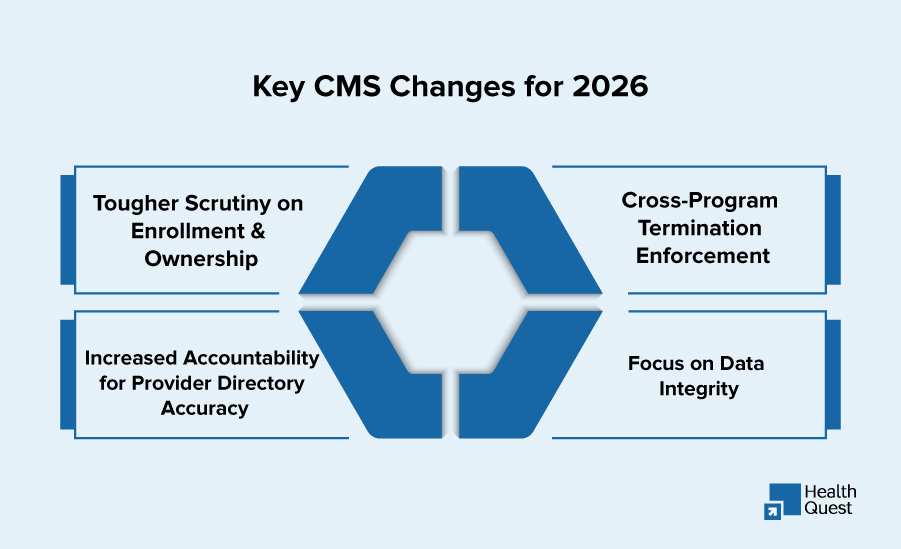
CMS has clearly outlined its enforcement priorities for 2026. These changes will affect healthcare providers in every specialty, from primary care to specialized treatment facilities. Here’s a breakdown of the key areas providers need to focus on:
1. Tougher Scrutiny on Enrollment and Ownership
CMS is intensifying its scrutiny over provider documentation, particularly for Skilled Nursing Facilities (SNFs), Home Health Agencies (HHAs), and Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) suppliers. The focus will be on ensuring that ownership and enrollment details are thoroughly documented and verified.
What Providers Need to Do:
- Providers must ensure that all ownership and enrollment details are accurate and aligned with CMS’s requirements.
- Implement processes to regularly review and verify data to avoid unnecessary errors during audits.
2. Cross-Program Termination Enforcement
Under the new rules, a termination from Medicare can trigger automatic terminations across Medicaid, CHIP, and other related programs. This creates a cascading effect, which could disrupt patient care and billing across multiple systems.
What Providers Need to Do:
- Healthcare organizations must closely monitor provider status across all programs.
- Providers should be aware of the potential for automatic terminations and ensure that their credentials are up-to-date across all programs.
3. Increased Accountability for Provider Directory Accuracy
Medicare Advantage (MA) plans are now under increased scrutiny when it comes to the accuracy of provider directories. While providers may not directly submit directory data to CMS, MA plans are responsible for ensuring the accuracy of this information. Failure to maintain correct provider directories could lead to audits, penalties, or exclusion from networks.
What Providers Need to Do:
- Ensure that directory information, including specialties and demographic data, is always up to date.
- Providers should coordinate with MA plans to maintain accurate directory information and address any discrepancies quickly.
4. Focus on Data Integrity
CMS is placing a heavier emphasis on maintaining accurate provider data, including identifiers, practice locations, ownership details, and effective dates. Credentialing teams and providers alike must take extra precautions to ensure that this data is accurate and current.
What Providers Need to Do:
- Regularly audit and update all provider data to ensure compliance with CMS’s stringent data integrity rules.
- Implement systems that allow for easy tracking and updating of provider data across various platforms.
How These Changes Will Affect Providers: Key Operational Shifts
As CMS regulations evolve, healthcare providers will need to shift from reactive compliance practices to proactive ones. These changes require an overhaul in how provider data is managed, reported, and updated. Below are some key operational shifts providers will face in 2026:
1. Medicare Fee-for-Service: PECOS as the Core System
CMS has reinforced that PECOS (Provider Enrollment, Chain, and Ownership System) will serve as the authoritative source of truth for Medicare enrollment data. Providers must ensure that PECOS data is consistently updated and aligned with internal systems to avoid errors.
Actionable Steps for Providers:
- Regularly update PECOS information and align it with other internal databases, such as NPPES.
- Be proactive in verifying provider data to prevent cascading errors in multiple payer systems.
2. Expanded Reporting Requirements: Timely Action is Critical
CMS is increasing the enforcement of existing reporting requirements. Providers must report adverse actions, ownership changes, and practice location updates within strict deadlines (typically 30 days). Failure to report on time will be considered a violation of CMS regulations and can result in severe penalties.
Actionable Steps for Providers:
- Ensure that all changes are documented and submitted within the required timeframe.
- Set up internal protocols to notify the credentialing team immediately of any changes that need to be reported to CMS.
3. Provider Directory Accuracy in Medicare Advantage
Medicare Advantage plans will face more rigorous audits regarding provider directory accuracy. Providers must ensure that their data is correctly listed and easily accessible for MA plans to maintain compliance.
Actionable Steps for Providers:
- Regularly review and update directory information to meet CMS’s accuracy standards.
- Work closely with MA plans to confirm that all data submitted is up-to-date and accurate.
4. Medicaid and CHIP: Cross-Termination Risk
CMS’s focus on cross-program terminations means that a provider’s termination in one program could trigger automatic terminations across multiple payers. Providers must ensure ongoing monitoring of their enrollment status to prevent unexpected disruptions.
Actionable Steps for Providers:
- Regularly track and manage terminations across all relevant payer systems.
- Implement a system for monitoring status changes to ensure that terminations in one program are addressed across others.
How Providers Can Stay Ahead of CMS Changes
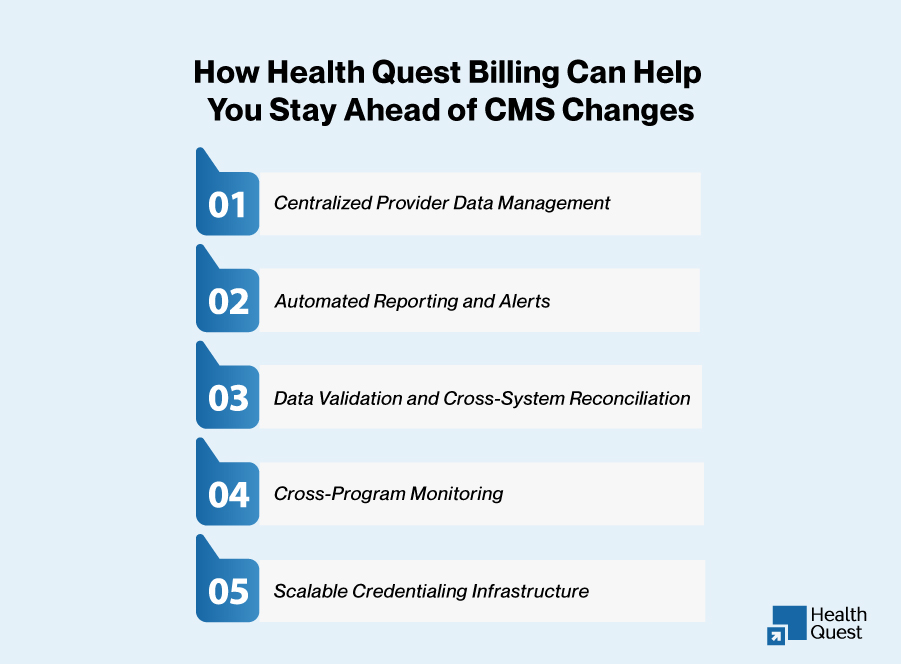
Given the increased complexity of CMS’s 2026 regulations, healthcare providers need a robust, automated system to streamline credentialing processes, stay compliant, and minimize risk. Health Quest Billing offers a comprehensive suite of tools to help providers navigate these challenges effectively.
Key Features of Health Quest Billing for Providers:
IMAGE TOPIC: How Health Quest Billing Can Help You Stay Ahead of CMS Changes
- Centralized Provider Data Management:
- Consolidates all provider data into a single, easily accessible platform, ensuring accuracy and alignment across systems like PECOS, NPPES, and internal credentialing tools.
- Automated Reporting and Alerts:
- Automates the process of reporting to CMS, ensuring providers meet all deadlines. Real-time alerts notify providers of necessary updates to ownership, practice locations, or adverse actions.
- Data Validation and Cross-System Reconciliation:
- Ensures real-time data validation and consistency between PECOS, NPPES, and internal systems, reducing errors and ensuring compliance with CMS requirements.
- Cross-Program Monitoring:
- Tracks provider status across all payers, ensuring that terminations, exclusions, and status changes are managed promptly, keeping providers compliant across all programs.
- Scalable Credentialing Infrastructure:
- As credentialing volumes increase, Health Quest Billing offers flexible workflows and scalable solutions to help providers manage growing credentialing demands efficiently.
Preparing for 2026: The Path Forward for Providers
To succeed in this new regulatory environment, healthcare providers must move beyond reactive credentialing practices and embrace automation, data accuracy, and timely reporting. Providers who stay ahead of CMS regulations will protect their revenue streams, reduce compliance risks, and ensure uninterrupted patient care.
Conclusion:
The CMS changes for 2026 present significant challenges for healthcare providers, but they also offer an opportunity to strengthen operational practices and ensure compliance with evolving regulations. By adopting the right tools and strategies, providers can ensure that their credentialing and data management processes meet CMS’s rigorous standards, reducing the risk of errors and protecting revenue streams.