Occupational therapy (OT) billing and coding is no longer just an administrative task; it’s a direct driver of revenue, compliance, and practice growth. As occupational therapy practices move into 2026, billing complexities are increasing, payer scrutiny is tightening, and outdated workflows are costing practices real money.
2025 was a tough year for many OT providers. Rising claim denials, Medicare reimbursement pressure, telehealth confusion, and constant CPT and ICD-10 code updates created financial strain across practices of all sizes. And unfortunately, many of those challenges haven’t disappeared; they’ve evolved.
The good news? OT practices that modernize their billing and coding strategy in 2026 can recover lost revenue, reduce denials, and stabilize cash flow.
Why Accurate Occupational Therapy Billing & Coding Matters
Occupational therapy billing and coding are the backbone of your revenue cycle management (RCM). Every evaluation, treatment session, and progress note must be translated into accurate CPT, ICD-10, and HCPCS codes to ensure proper reimbursement. For many practices, partnering with professional medical billing services has become essential to keep this process accurate, compliant, and efficient.
Even minor errors can lead to:
- Claim denials: Incorrect codes or incomplete documentation result in claims being rejected.
- Payment delays: Mistakes in coding delay reimbursement, leaving your practice struggling to cover operational costs.
- Reduced reimbursement: Inaccurate codes may cause you to receive less than you’re entitled to.
- Compliance audits: Improper billing practices increase the risk of audits, putting your practice’s reputation and finances at risk.
- Lost revenue: The failure to bill accurately for all services performed means that money rightfully owed to you is lost.
With Medicare and Medicare Advantage increasing scrutiny, clean claims and airtight documentation are no longer optional.
Accurate OT billing and coding ensures:
- Faster reimbursements
- Lower denial rates
- Regulatory compliance
- Predictable cash flow
- Financial stability
This makes the billing process not just an administrative task but a critical revenue driver.
Top Occupational Therapy Billing Challenges Practices Faced in 2026
1. Rising Claim Denial Rates
Denials were one of the biggest revenue disruptors for occupational therapy practices in 2025 and they remain a top concern in 2026.
Common denial triggers included:
- Coding errors: Incorrect CPT or ICD-10 codes, or using outdated codes, are one of the leading causes of claim rejections. Even a small typo can trigger a denial, costing you time and revenue.
- Medical necessity gaps: Insurance companies now demand more robust documentation to justify medical necessity. This means that if the need for the service isn’t clearly established, the payer won’t approve the reimbursement.
- Modifier misuse: Modifiers such as -25 (separate, significant service) and -59 (distinct procedural service) are often misunderstood or misused. When modifiers aren’t applied correctly, claims are flagged as errors and denied.
Each denied claim means lost time, delayed revenue, and the extra burden of administrative work to correct and resubmit the claim.
2. Medicare & Medicare Advantage Billing Complexities
Medicare continues to be a major payer for occupational therapy services but also one of the most challenging. The complexity of billing Medicare and Medicare Advantage plans in 2025 left many practices frustrated and financially stretched.
Key pain points from 2025:
- Medicare Physician Fee Schedule adjustments: Reimbursement for OT services under Medicare has been subject to annual fee schedule updates, which can result in reduced payment for some services.
- Lower reimbursement rates: Medicare reimbursement rates for OT services often fail to match the rising costs of delivering care, making it more challenging to stay profitable.
- Medicare Advantage plans with inconsistent rules: Each Medicare Advantage plan has different prior authorization requirements, eligibility guidelines, and billing codes, leading to confusion and delayed reimbursements.
- Confusing prior authorization requirements: Certain OT services require prior authorization, and practices that fail to navigate this complicated process risk claims being denied.
For many OT practices, navigating Medicare billing requirements without expert support resulted in delayed payments, lost revenue, and a significant administrative burden.
3. Telehealth Billing & Documentation Issues
Telehealth surged during the pandemic, and many OT practices continued to offer remote services in 2025. However, telehealth billing for OT services has remained a pain point due to frequent policy changes and inconsistencies in reimbursement.
Challenges OT practices faced:
- Constantly changing CMS telehealth rules: The Centers for Medicare & Medicaid Services (CMS) continually updated telehealth guidelines, making it difficult for OT providers to stay on top of new requirements.
- Limited coverage for certain OT services: Not all OT services are reimbursed when provided via telehealth, and certain types of telehealth care require more stringent documentation.
- Missing or insufficient virtual visit documentation: Telehealth claims that lack the required documentation are more likely to be denied, leaving OT practices with unpaid claims.
- Incorrect telehealth modifiers and place-of-service codes: Without a proper understanding of the telehealth-specific codes and modifiers, claims can be rejected or underpaid.
Without proper telehealth billing workflows, many OT practices saw claims denied despite delivering valid care.
4. Frequent CPT & ICD-10 Code Updates
CPT and ICD-10 codes change frequently, and OT practices often struggle to keep up with these updates. New codes are introduced, and old ones are retired, which can lead to billing errors if practices don’t implement the necessary changes quickly enough.
Impact on OT services:
- OT evaluations, treatments, and therapeutic interventions each have specific codes. Failing to update billing systems with new codes can lead to incorrect claims and revenue leakage.
- Practices that didn’t train staff or update software systems quickly enough faced inaccurate claims and denied reimbursements.
How Occupational Therapy Practices Can Overcome Billing Challenges in 2026
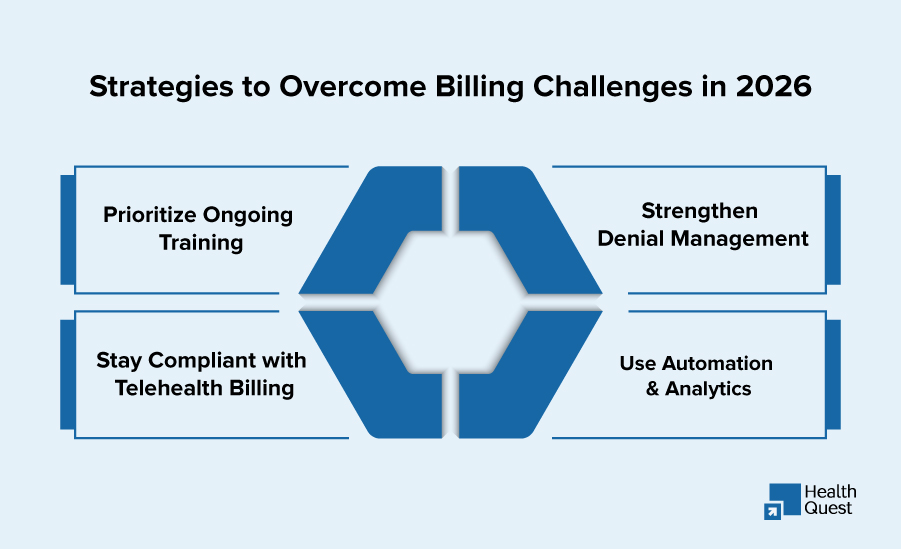
While many challenges persist, there’s a clear path to overcoming them in 2026. OT practices can position themselves for success by adopting best practices and modernizing their billing systems.
1. Prioritize Ongoing Billing & Coding Training
The key to reducing errors and staying on top of complex billing requirements is regular, ongoing education.
Best practices for 2026:
- CPT & ICD-10 training: Regularly update your team on the latest coding changes and nuances.
- Medicare billing refreshers: Ensure that staff understand the specific nuances of Medicare billing.
- Modifier usage education: Train staff on the correct application of modifiers to avoid mistakes.
- Documentation compliance workshops: Ensure that every piece of documentation is sufficient to justify the service and demonstrate medical necessity.
Regular training will reduce errors, improve clean claim rates, and help your practice stay compliant.
2. Strengthen Denial Management Processes
Denial management is crucial to improving cash flow and minimizing revenue loss. OT practices must have a structured, proactive denial management system in place to track and address denied claims.
Winning strategies include:
- Track denial trends by payer: Use data analytics to identify patterns in denials. This helps practices spot recurring issues.
- Identify root causes: Whether it’s coding errors, lack of documentation, or payer-specific issues, addressing the root causes will help prevent future denials.
- Appeal denied claims promptly: Develop a process for quickly appealing denied claims and resubmitting them with the correct information.
- Prevent repeat errors with claim scrubbing: Implement claim scrubbing tools to catch errors before claims are submitted.
A proactive denial management strategy can significantly reduce claim rejections and recover thousands in lost revenue.
3. Stay Compliant With Telehealth Billing Rules
Telehealth isn’t going anywhere but it requires precision.
OT practices must:
- Stay updated on CMS telehealth policies: Ensure your practice stays current with CMS guidelines for telehealth.
- Use correct telehealth CPT codes and modifiers: Ensure that your practice applies the right codes for telehealth services, and that you are using the correct place-of-service codes.
- Ensure virtual visit documentation meets in-person standards: CMS and other payers require that telehealth documentation be just as detailed as in-person visits.
- Verify payer-specific telehealth coverage: Confirm that each payer covers telehealth OT services, as policies can vary widely.
By staying compliant, your practice will improve reimbursement rates for telehealth.
4. Use Automation & Revenue Analytics
Manual billing processes increase errors and slow payments. In 2026, smart OT practices are leveraging:
- Automated claim scrubbing: Prevent billing errors by using automation to scrub claims for accuracy before submission.
- Electronic claim submission: Streamline your claims process by using electronic submissions, reducing paperwork and accelerating payment
- Real-time denial tracking: Use software to track denials in real-time, so your team can act quickly to resolve issues.
- Revenue cycle analytics dashboards: Track key metrics such as denial rates, claim statuses, and payer performance.
Automation and analytics improve efficiency and provide real-time insight into where revenue is being lost and how to fix it.
Occupational Therapy Coding Cheat Sheet
| Code Type | Code | Description |
| CPT | 97165 | OT Evaluation – Low Complexity |
| CPT | 97166 | OT Evaluation – Moderate Complexity |
| CPT | 97167 | OT Evaluation – High Complexity |
| CPT | 97530 | Therapeutic Activities |
| CPT | 97535 | Self-Care/Home Management Training |
| CPT | 97112 | Neuromuscular Re-education |
| CPT | 97150 | Group Therapy |
| ICD-10 | M62.81 | Muscle Weakness (Generalized) |
| ICD-10 | F82 | Developmental Coordination Disorder |
| ICD-10 | G81.90 | Hemiplegia |
| Modifier | -25 | Significant, Separate Service |
| Modifier | -59 | Distinct Procedural Service |
How Health Quest Billing Helps OT Practices Thrive in 2026
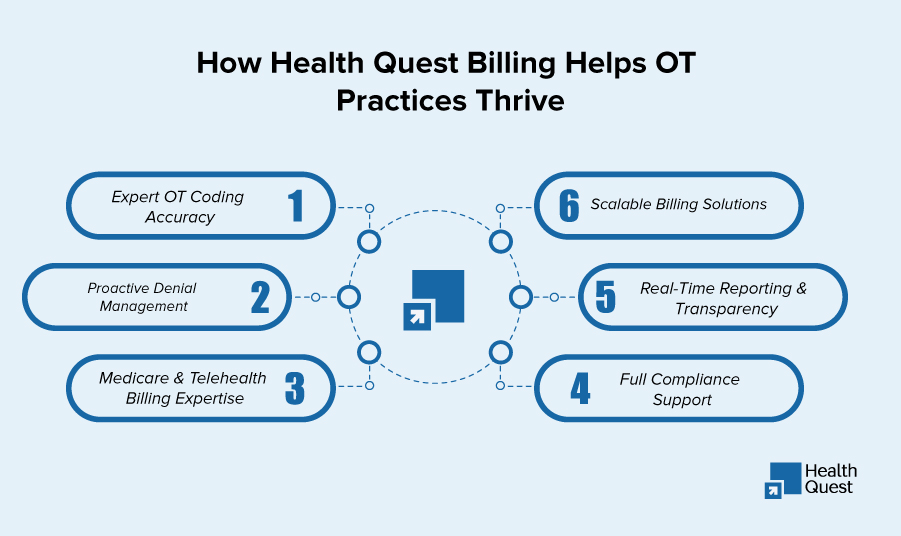
Health Quest Billing provides specialized occupational therapy billing and coding services tailored to the unique needs of OT practices. Our services are designed to eliminate denials, improve compliance, and maximize revenue, ensuring your practice can focus on what matters most patient care.
What Sets Us Apart:
-
Expert OT Coding Accuracy
We stay up-to-date with 2026 CPT, ICD-10, and Medicare updates, ensuring every service provided is accurately coded. This attention to detail minimizes billing errors and ensures you’re reimbursed appropriately for the care you provide.
-
Proactive Denial Management
We thoroughly scrub claims before submission to catch errors early, reducing the chance of denials. When denials do occur, we manage the appeal process swiftly, so your practice can recover lost revenue without unnecessary delays.
-
Medicare & Telehealth Billing Expertise
Navigating Medicare’s complex billing structure and staying compliant with telehealth requirements can be a hassle. At Health Quest, we handle Medicare billing intricacies and ensure your telehealth services are fully compliant with the latest regulations, maximizing your reimbursement opportunities.
-
Scalable Billing Solutions
Whether you’re a solo OT practitioner or part of a multi-location practice, our services are designed to scale with your needs. From single-provider billing to complex, multi-site operations, we provide tailored solutions that grow with your practice.
-
Real-Time Reporting & Transparency
With our real-time reporting dashboards, you get full transparency into your practice’s financial health. Track claims status, denial rates, and payer performance in real time, allowing you to make informed decisions that drive profitability and efficiency.
-
Full Compliance Support
We ensure your practice stays on top of CMS updates, payer-specific regulations, and changing healthcare policies. With our full compliance support, we handle regulatory changes, so you never have to worry about missing critical updates that could impact your reimbursement.
Conclusion:
Occupational therapy billing and coding challenges didn’t stop in 2025, but 2026 offers a chance to reset, optimize, and grow.
By improving documentation, strengthening denial management, staying compliant with Medicare and telehealth rules, and partnering with experts like Health Quest Billing, OT practices can:
- Reduce denials
- Improve cash flow
- Stay compliant
- Focus on patient care not paperwork
Ready to future-proof your occupational therapy billing?
Health Quest Billing is here to help your practice thrive in 2026 and beyond.