You can deliver exceptional ABA care and still struggle with cash flow, and billing is usually the reason. As demand for ABA therapy increases, billing rules become more complex, denials become more frequent, and payments become more unpredictable. ABA billing isn’t just paperwork; it’s one of the biggest factors affecting your practice’s financial health.
At Health Quest Billing, we deal with these challenges every day. In this blog, we’ll explain what makes ABA billing unique, the most common mistakes providers face, and how specialized billing support can turn billing from a headache into a growth strategy.
What is ABA Therapy and Why Does It Require Specialized Billing?
ABA therapy is a therapeutic approach used to improve specific behaviours and skills, particularly for individuals on the autism spectrum. It includes various services such as:
- Behavior Assessments
- Therapeutic Interventions
- Parent and Caregiver Training
- Supervision by BCBAs (Board-Certified Behavior Analysts)
The wide range of services in ABA therapy requires a variety of billing codes and documentation processes, which can be overwhelming for providers without specialized knowledge. Missteps in coding or billing could lead to claim denials, underpayments, and disruptions in revenue streams.
Common Challenges in ABA Therapy Billing
Navigating the billing process for ABA therapy can be complex, and providers face unique challenges that can hinder the financial health of their practice. Below are some common issues ABA providers encounter:
-
Variety of Service Codes for Different Therapy Types
ABA therapy consists of several distinct types of services, each with its own set of billing codes. This can be confusing for practices without an expert billing team who can track the correct codes for each service.
-
Complex Insurance Requirements
Insurance providers often have different requirements for covering ABA therapy services, and these requirements can change frequently. Some insurers may cover assessments but not therapy, while others may have limitations on the number of therapy hours covered.
-
Documentation and Medical Necessity
Proper documentation of medical necessity is critical for ABA therapy claims. Failure to properly document the justification for therapy services often leads to claim denials. This is particularly relevant for assessments, parent training, and ongoing therapy.
-
Constantly Changing Billing Codes
ABA therapy billing codes can change periodically, making it crucial for providers to stay updated. Incorrect or outdated codes can lead to denials or reduced reimbursement rates.
- Supervision and Overseeing Requirements
ABA therapy often requires supervisory oversight by a BCBA, and these services have their own set of coding and billing requirements. Misunderstanding the rules about supervision can lead to underpayments or delays in reimbursement.
The Importance of Accurate Coding for ABA Therapy
Coding is the backbone of ABA therapy billing, and accurate coding ensures that your practice gets reimbursed appropriately. The following are some of the most frequently used CPT and HCPCS codes for ABA therapy:
- 97151: Behavior identification assessment
- 97153: Adaptive behavior treatment by protocol
- 97154: Group adaptive behavior treatment
- H2019: Therapeutic behavioral services
Properly applying the correct codes for each service helps ensure that your practice is compensated fairly and accurately. Misuse of codes or failure to update to the latest codes can lead to delays in payment or outright claim rejections.
Common ABA Therapy Billing Errors and How to Avoid Them
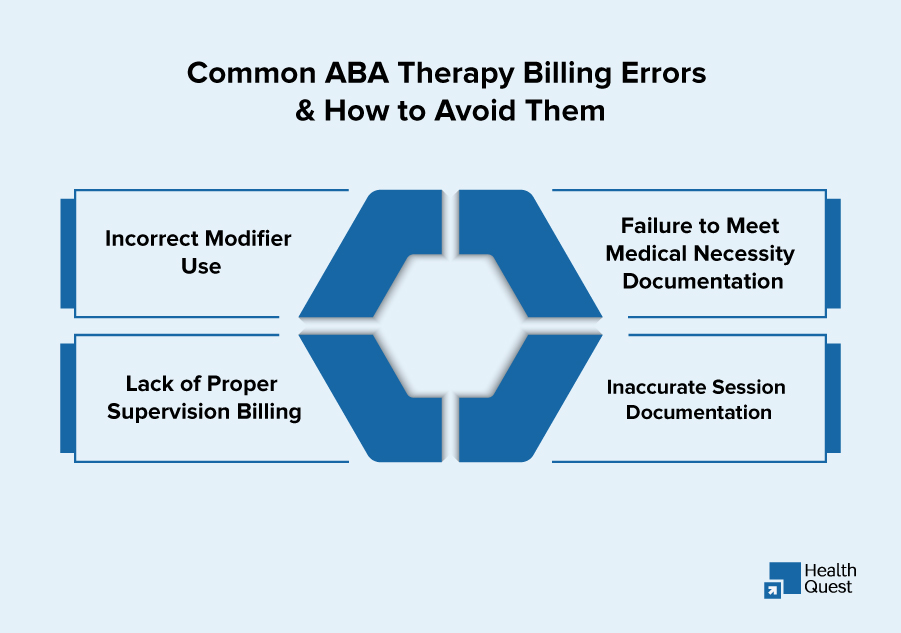
There are several common errors that can negatively affect your practice’s revenue cycle. Let’s explore some of the most frequent mistakes:
1. Incorrect Modifier Use
Modifiers such as -25, -59, or -XU are necessary to indicate that multiple procedures were performed on the same day. Incorrect modifier application can cause claims to be rejected or underpaid.
2. Failure to Meet Medical Necessity Documentation
For ABA therapy services to be reimbursed, providers must document why the service is medically necessary. Insufficient documentation or vague notes can trigger denials.
3. Lack of Proper Supervision Billing
Supervision by a BCBA (Board-Certified Behavior Analyst) is required for many ABA services, but these hours are often underbilled or not properly tracked. This leads to missed revenue opportunities.
4. Inaccurate Session Documentation
Detailed session notes are necessary to demonstrate the clinical need for services. Incomplete or inaccurate documentation can result in the inability to prove medical necessity during audits or claims review.
Cheat Code for ABA Therapy Billing: Key Codes, Modifiers, and Tips
| Billing Element | Code | Description | Tip for Accurate Billing |
| Behavior Identification Assessment | 97151 | Used for the initial or ongoing assessment of behavior. | Ensure that the assessment includes a detailed evaluation of target behaviors, goals, and treatment plans. |
| Therapeutic Behavioral Services | H2019 | Used for therapeutic behavioral interventions provided by a technician. | Always document the specific interventions used and the goals of therapy for accurate reimbursement. |
| Adaptive Behavior Treatment | 97153 | Adaptive behavior treatment by protocol, delivered by a behavior technician. | Include session notes that outline specific behaviors addressed and progress toward treatment goals. |
| Group Adaptive Behavior Treatment | 97154 | Group-based adaptive behavior treatment. | Be clear about the group size and specific goals worked on during the session. |
| Behavior Technician Services | 97155 | Services provided by a BCBA or qualified professional, often used in direct therapy. | Ensure that service time is divided between technician and BCBA when billing. |
| Parent Training and Education | 97156 | Training for caregivers to reinforce behavior modification techniques. | Document the caregiver’s role in reinforcing the skills learned and how it’s integrated into daily routines. |
| Supervision by BCBA | 97158 | Supervision of ABA therapy provided by a Board-Certified Behavior Analyst (BCBA). | Separate out BCBA supervision from therapy time and ensure that the BCBA’s supervision hours are correctly billed. |
| CPT Modifiers | -25 | Used for a significant, separately identifiable Evaluation and Management (E/M) service. | Apply when an E/M service is provided in conjunction with therapy on the same day. |
| CPT Modifiers | -59 | Distinct procedural service modifier used for separate procedures. | Use carefully when multiple procedures are billed during the same encounter to avoid bundling issues. |
| CPT Modifiers | -XU | Used for “Unusual non-overlapping service” when two services do not overlap in content. | Best used when two different therapy sessions or interventions occur independently but in the same visit. |
| HCPCS Modifiers | -QX | For therapy services provided by a behavior technician under supervision. | Correctly document that the technician worked under supervision, which is a critical aspect of ABA billing. |
| Behavioral Health Assessment | 96156 | General behavioral health assessments used in ABA. | Ensure detailed documentation for the reason behind the assessment, patient diagnosis, and targeted behavior. |
Additional Tips for Successful ABA Therapy Billing
- Stay Current on Coding Changes: The codes used in ABA therapy are updated periodically, so it’s important to stay informed about the latest changes in the CPT and HCPCS codes.
- Proper Documentation is Key: Without clear documentation of medical necessity and session specifics, claims are often denied. Always include the reason for therapy, goals, and detailed session notes.
- Use Correct Modifiers: Modifiers like -25, -59, and -XU play a significant role in getting claims paid correctly. Be sure to use these modifiers only when necessary and based on payer guidelines.
- Separate Supervision and Therapy Hours: ABA therapy often includes supervision by a BCBA. Make sure supervision hours are billed separately from direct therapy time to avoid underpayment.
- Ensure Accurate Time Reporting: Some ABA therapy services, especially those involving supervision or group therapy, require specific time-based billing. Ensure that every minute of service is reported accurately, as even a slight mistake can lead to revenue loss.
How Health Quest Billing Can Help Streamline ABA Therapy Billing

At Health Quest Billing, we specialize in ABA therapy billing and coding services. Our goal is to simplify the billing process, reduce denials, and ensure that your practice receives accurate reimbursements. Here’s how we can help:
1. Expert Coding and Billing
We use the correct CPT and HCPCS codes for each ABA therapy service, ensuring that you’re always paid for the services rendered. Our team stays up to date with the latest code changes to avoid billing errors.
2. Handling Insurance Variability
Health Quest Billing has extensive experience working with multiple insurance providers. We ensure that we comply with each payer’s specific requirements to prevent rejections and underpayments.
3. Streamlined Denial Management
If your claims are denied, we don’t stop there. Our team will work quickly to resolve the issue, appealing any denials and reworking claims to ensure timely reimbursement.
4. Comprehensive Documentation Support
We guide your team in maintaining detailed, compliant documentation that justifies the medical necessity of each ABA therapy service. This reduces the chances of denials and audits.
5. Transparent Reporting
Our services provide you with clear, easy-to-understand reports on your revenue cycle, helping you track claim status and payment trends, so you can make more informed decisions.
The Impact of Proper ABA Therapy Billing on Your Bottom Line with Health Quest Billing
When ABA therapy billing is managed effectively by Health Quest Billing, your practice can experience a transformative shift in financial health, operational efficiency, and patient satisfaction. Here’s what your practice can expect after partnering with us:
- Reduced Claim Denials
- Maximized Reimbursement
- Faster Payment Processing
- Lower Administrative Burden
- Enhanced Compliance and Audit Protection
- Improved Financial Reporting and Insights
- Proactive Denial Management and Appeal Handling
- Streamlined Billing for Telehealth Services
Key Trends Shaping ABA Therapy Billing and Coding in 2026
The ABA therapy landscape continues to evolve, and staying ahead of changes is crucial for maintaining a healthy revenue cycle. Some upcoming trends include:
Expanded Coverage for ABA Services
- More insurance plans are expanding coverage for ABA therapy services, including assessments and caregiver training.
- Providers must stay updated on payer-specific requirements for these expanded services.
Increased Utilization of Telehealth
- Telehealth for ABA therapy will continue to grow, with more insurers offering coverage.
- Providers need to understand new codes and payer rules for virtual sessions.
Data-Driven Billing Solutions
- AI and data analytics will play a larger role in billing accuracy, underpayment tracking, and payer insights.
- Automation will streamline workflows, improving revenue cycle management.
Value-Based Care Models
- Payers will focus more on therapy outcomes rather than volume of services.
- Providers must integrate patient progress data with billing to meet value-based care standards.
Cross-State and Multidisciplinary ABA Services
- ABA providers will serve patients across multiple states, requiring compliance with varying payer policies.
- Understanding state-specific Medicaid and insurance rules will be crucial for billing.
Conclusion: Protect Your ABA Therapy Revenue with Health Quest Billing
Accurate billing and coding are fundamental to ensuring that your ABA therapy services are reimbursed correctly and on time. At Health Quest Billing, we specialize in managing the unique billing needs of ABA therapy providers, helping you avoid costly errors and increasing your revenue potential.
If you’re ready to streamline your billing process, reduce denials, and maximize reimbursement, contact Health Quest Billing today for a consultation. Let us help you optimize your revenue cycle and focus on what you do best—delivering high-quality care to your patients.