Internal medicine practices are struggling with skyrocketing AR days, especially in high-demand states like California, Texas, and New York. As payer policies become more complex and Medicare regulations tighten, many practices are seeing payment delays that last 45–90 days, crippling cash flow and stalling growth. These extended delays not only reduce financial flexibility but also increase operational strain. In 2026, if your practice doesn’t streamline its revenue cycle management (RCM), you’re leaving vital revenue on the table. It’s time to tackle AR head-on and ensure quicker, more reliable payments to keep your practice thriving.
Understanding AR Days and Their Impact on Internal Medicine Practices
AR days are a key metric in healthcare billing. They represent the average number of days between providing a service and receiving payment. The longer AR days are, the slower the cash flow, which affects practice operations, payroll, and the ability to reinvest in new technologies or hire additional staff.
For internal medicine practices, high AR days are often a result of:
- Complex payer requirements, including Medicare, Medicaid, and commercial insurance plans.
- Slow payer response times, which can stretch claims approval cycles.
- Inconsistent patient collections, particularly when patients are responsible for large co-pays or deductibles.
- Coding errors and incomplete documentation, which result in claim rejections and resubmissions.
Why Reducing AR Days is Crucial in 2026
The ability to reduce AR days in 2026 is essential for improving your practice’s cash flow and overall financial health. Here are some key reasons why managing AR is so critical:
- Cash Flow Stability: The longer the AR days, the less money available for day-to-day operations. Practices that experience slow payments risk the ability to pay bills on time and invest in new technologies or staffing.
- Profitability: High AR days indicate inefficiencies in the billing process, which translates to higher administrative costs due to repeated follow-ups, claims resubmissions, and appeals.
- Operational Efficiency: AR issues take valuable time away from patient care. Practice staff spend a significant portion of their time tracking down payments instead of focusing on delivering exceptional patient care.
According to 2025 data from the American College of Physicians (ACP), practices that reduce their AR days to below 45 days experience improved financial performance and have more predictable cash flow, allowing them to scale their services and hire additional staff.
Top Challenges Contributing to Extended AR Days in Internal Medicine Practices
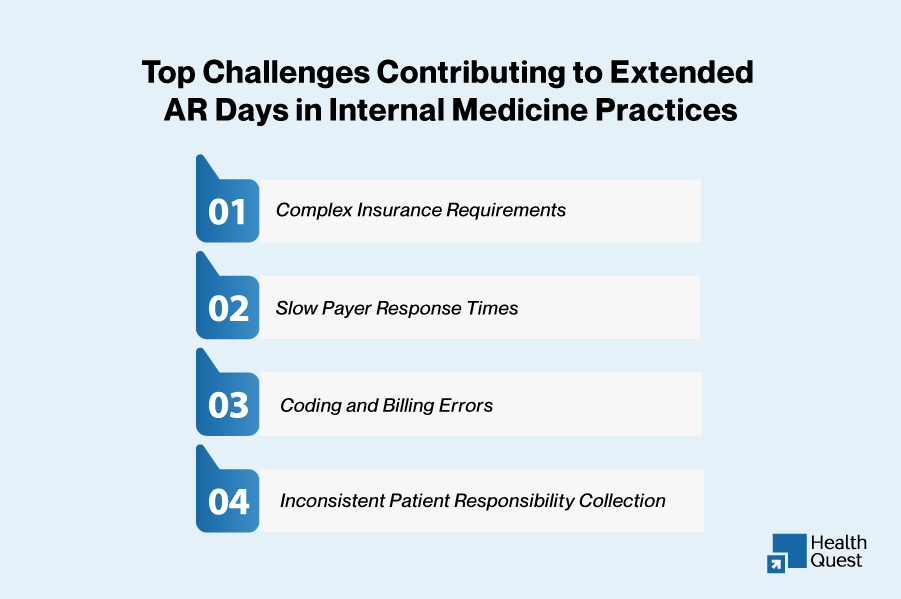
There are several factors that contribute to long AR cycles in internal medicine practices. Below are some of the most significant challenges:
1. Complex Insurance Requirements
Internal medicine practices often deal with multiple payers, including government programs like Medicare, Medicaid, and commercial insurance. Each payer has its own set of requirements, including unique CPT codes, ICD-10 codes, and prior authorization processes. This complexity can lead to delayed approvals, claim rejections, and ultimately, longer AR days.
2. Slow Payer Response Times
The average payer response time in 2026 is expected to increase due to stricter regulations and more rigorous audits. Practices that rely on manual submission and follow-up processes may find themselves waiting weeks or months to receive payment, which prolongs the AR cycle.
3. Coding and Billing Errors
Internal medicine involves a wide variety of services, from routine office visits to complex diagnostic testing. Coding errors, such as incorrect or missing modifiers, incorrect CPT code selection, and incomplete ICD-10 codes, often lead to claim denials or delayed payments. Even small coding errors can significantly extend AR days.
4. Inconsistent Patient Responsibility Collection
High deductibles and co-pays have become common in many insurance plans. Collecting these payments at the point of service can be challenging, especially if patients are unaware of their financial responsibilities. Delayed or missed collections from patients contribute to longer AR days.
How to Reduce AR Days in Internal Medicine Practices in 2026
Reducing AR days requires a multi-faceted approach that involves streamlining billing processes, improving coding accuracy, and adopting proactive strategies for collections and denials management. Below are some strategies that can help internal medicine practices achieve faster reimbursements:
1. Streamline the Eligibility and Authorization Process
A significant portion of AR delays in internal medicine practices can be attributed to insurance eligibility verification and prior authorization issues. Automating these processes can significantly reduce AR days by ensuring that eligibility and prior authorizations are confirmed before services are provided.
- Automated Eligibility Verification: Use tools to verify patient eligibility in real-time before services are rendered. This can help eliminate surprise denials due to lack of coverage.
- Automated Prior Authorization Requests: Ensure all necessary prior authorizations are completed in advance of procedures to avoid unnecessary delays in claim approvals.
2. Improve Coding Accuracy and Documentation
Ensuring that all procedures and diagnoses are correctly coded is critical in reducing AR days. Inaccurate coding leads to denied claims and longer resubmission times.
- Train Coders Regularly: Ensure that coding teams stay up-to-date with the latest CPT codes and ICD-10 codes specific to internal medicine.
- Standardize Documentation: Implement standardized templates to ensure that medical necessity is always documented thoroughly.
3. Implement Proactive Denial Management
Denial management is one of the most effective ways to reduce AR days. Tracking denials in real-time, identifying the root causes, and resubmitting claims promptly are key steps in reducing payment delays.
- Track Denied Claims Immediately: Implement a system for tracking denied claims and initiate an appeal process within 24–48 hours of denial.
- Automated Appeals Process: Automate the creation and submission of appeals to streamline the process and reduce AR days.
4. Optimize Patient Payment Collections
Internal medicine practices can significantly reduce AR days by improving how they collect payments from patients.
- Collect Co-pays Upfront: Make it a practice to collect co-pays and deductibles at the time of the visit to reduce outstanding balances.
- Use Online Payment Portals: Offer patients an easy, online method to pay their bills, reducing delays in collections.
- Flexible Payment Plans: For patients with high-deductible plans, offer payment plans to ensure that balances are paid off promptly.
5. Leverage Technology for AR Tracking and Analytics
Using data analytics tools can give you greater visibility into your AR performance. This allows your practice to identify trends and problem areas before they become major issues.
- Track AR Aging: Use cloud-based systems to monitor AR aging in real-time, allowing you to address aging claims before they exceed 90 days.
- Payer Performance Monitoring: Track which payers are taking longer to process claims and adjust your follow-up process accordingly.
Emerging Trends in Internal Medicine AR Management in 2026
| Trend | Traditional Practice | Impact on AR | Best Practice |
| AI Billing Automation | Manual claim tracking | Slow payments, higher AR days | Leverage AI for real-time denials tracking and automation |
| Telehealth Billing Growth | Manual telehealth coding | Claim rejections, payment delays | Standardize telehealth billing rules and coding |
| High-Deductible Plans | Poor upfront collections | Higher patient balances | Collect payments upfront or offer payment plans |
| Online Patient Payments | Paper billing, mailed invoices | Delayed payments, low collections | Use patient portals for quicker, easier payments |
| Outsourced AR Services | In-house billing teams | Slow AR recovery, resource strain | Outsource to RCM experts for faster results |
| EHR-Billing Integration | Disconnected systems | Coding errors, delays in billing | Use integrated EHR systems for seamless billing |
| Medicare & Medicaid Compliance | Inconsistent tracking of requirements | Claim denials and slow payments | Automate compliance tracking and prior authorizations |
Key AR Metrics Internal Medicine Practices Must Track in 2026
Tracking the right performance indicators allows practices to identify trends, diagnose problems early, and accelerate revenue recovery. Below are essential AR metrics every internal medicine practice should monitor:
| Metric | 2026 Benchmark | Goal |
| Average AR Days | 30–40 days | Reduce below 40 (top practices aim for <35) |
| AR Aging >90 Days | <10–15% of total AR | Minimize delayed payments |
| Clean Claim Rate | 90%+ | Reduce rework & denials |
| Denial Rate by Payer | <5% | Track and optimize payer performance |
| First‑Pass Claim Acceptance | 85–90% | Maximize first‑time payment |
| Patient Responsibility Collection | 80–95% | Improve upfront and point‑of‑service collections |
These metrics provide a clear, data‑driven view of your practice’s revenue cycle performance. Monitoring them consistently allows practices to tackle bottlenecks before they turn into costly, long‑standing AR issues.
Why These Best Practices and Metrics Matter for Internal Medicine
Internal medicine practices often juggle a broad range of services from preventive care and chronic disease management to urgent visits and routine screenings. Each of these encounters generates clinical documentation and billing data that must be processed accurately and efficiently. When practices ignore AR metrics or rely on reactive billing workflows, they risk:
- Slow cash flow that squeezes operational liquidity
- Increased administrative costs due to unresolved denials and resubmissions
- Diminished ability to invest in care delivery or technology
- Higher write‑offs from accounts that age beyond payer filing deadlines
According to revenue cycle experts, many high‑performing healthcare organizations aim to keep AR Days under 40 and maintain less than 15% of AR in the >90‑day bucket to protect financial stability and operational agility.
How Health Quest Billing Can Help Internal Medicine Practices Reduce AR Days
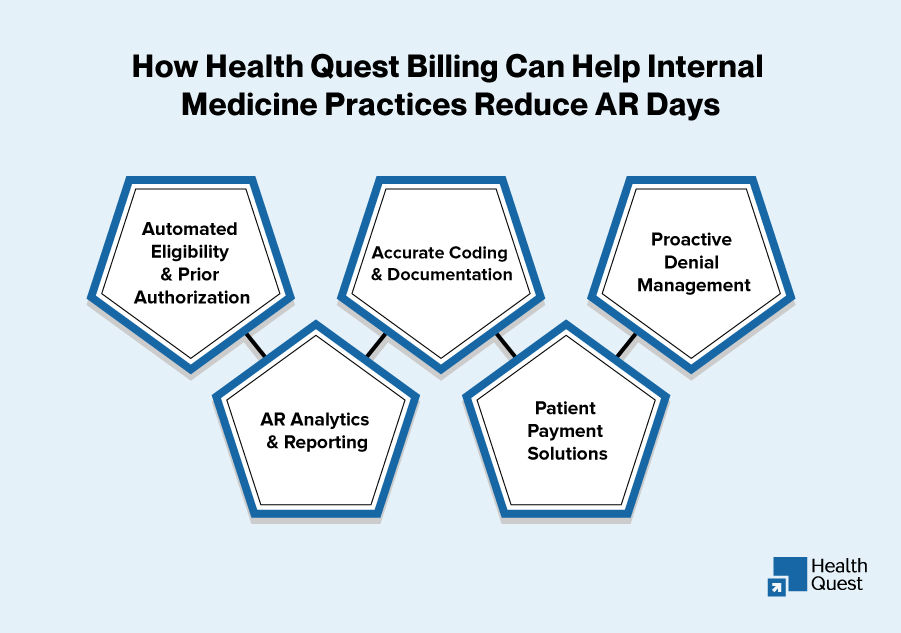
At Health Quest Billing, we specialize in internal medicine billing and AR management solutions. Our services are designed to help practices reduce AR days, improve cash flow, and maximize revenue.
- Automated Eligibility & Prior Authorization: We handle real-time eligibility checks and prior authorization requests, ensuring that your practice is always prepared before providing services.
- Accurate Coding & Documentation: Our expert coders ensure that all claims are submitted with the correct codes and comprehensive documentation, minimizing the risk of denials.
- Proactive Denial Management: With automated denial tracking and swift appeals processes, we ensure that denied claims are quickly addressed, reducing downtime and accelerating payment cycles.
- AR Analytics & Reporting: Our cloud-based solutions offer real-time AR tracking and data analytics, providing your practice with the insights needed to optimize your revenue cycle.
- Patient Payment Solutions: We streamline patient collections by offering online payment portals and flexible payment plans, ensuring quicker payments and fewer outstanding balances.
By partnering with Health Quest Billing, your practice can experience up to a 35% reduction in AR days, faster payer response times, and improved revenue predictability in 2026.
Conclusion:
Reducing AR days is not only about improving cash flow but it’s also about optimizing your revenue cycle to support growth, reinvestment in technology, and ultimately, better patient care. In 2026, internal medicine practices must take a proactive approach to billing and AR management by adopting automation, improving coding accuracy, and implementing effective denial management strategies.
Health Quest Billing offers tailored solutions for internal medicine practices to reduce AR days, streamline operations, and boost profitability. Let us handle your AR management, so you can focus on providing exceptional care to your patients.