The 2026 Medicare Physician Fee Schedule isn’t just an update; it’s a wake-up call. For cardiology, orthopedics, and radiology practices, it signals one thing clearly: billing mistakes and inefficiencies will now hit your bottom line harder than ever. Procedural care is under tighter reimbursement rules, and relying on volume alone to cover gaps is no longer an option.
Medicare remains the largest revenue driver for most specialty practices, and even commercial payers often follow its lead. That means the 2026 PFS doesn’t just affect Medicare claims; it sets the tone for your entire revenue cycle, increasing denial risk, delaying payments, and putting pressure on cash flow if billing isn’t precise.
Understanding the 2026 Medicare Physician Fee Schedule and Its Impact on Specialty Billing
CMS’s Strategic Shift Away From Procedural Volume
The 2026 Medicare Physician Fee Schedule continues CMS’s multi-year strategy to rebalance spending away from volume-driven procedural medicine and toward care coordination, evaluation, and prevention. While this shift aligns with broader value-based care initiatives, it creates disproportionate challenges for specialties whose services are inherently procedural, technology-intensive, and resource-heavy.
Cardiology, orthopedics and radiology practices have not seen a corresponding reduction in clinical complexity or operational burden. Procedures still require advanced equipment, specialized clinical teams, strict regulatory oversight, and extensive documentation. However, CMS reimbursement assumptions increasingly reflect a belief that these services can be delivered more efficiently, even when real-world conditions suggest otherwise.
From a billing perspective, this disconnect increases financial risk. When reimbursement is compressed, practices lose the buffer that once offset minor coding errors, delayed submissions, or partial denials. In 2026, every claim must be defensible, compliant, and accurately supported at the time of submission.
Why “Small” Reimbursement Changes Have Large Financial Consequences
Many practices underestimate the cumulative impact of modest percentage reductions. A two- or three-per-cent cut to high-volume services compounds over the course of a year. When paired with underpayments, denials, or delayed reimbursement, these reductions can result in six-figure revenue losses for mid-sized specialty practices.
The 2026 PFS also increases the importance of understanding payer behavior beyond published rates. Medicare Advantage plans, in particular, are applying stricter authorization rules, narrower medical necessity interpretations, and more aggressive denial tactics. Billing teams must now manage not only CMS policy changes but also payer-specific variations that further complicate reimbursement.
Cardiology Billing After the 2026 Medicare Physician Fee Schedule
Increased Scrutiny of Diagnostic and Interventional Services
Cardiology remains one of the most Medicare-dependent specialties due to the prevalence of cardiovascular disease in aging populations. However, under the 2026 PFS, cardiology billing faces heightened scrutiny across both diagnostic and interventional services.
CMS has refined valuation models for cardiology procedures based on assumptions of improved efficiency and technological advancement. In practice, cardiology groups are experiencing the opposite: longer patient visits, more complex cases, increased documentation requirements, and staffing challenges that drive up operational costs.
Billing teams must now ensure that cardiology claims clearly demonstrate medical necessity, clinical decision-making, and procedural justification. Diagnostic tests, imaging studies, and repeat procedures are especially vulnerable to denials when documentation does not explicitly support why services were required and how they influenced patient care.
Coding Precision and Modifier Accuracy in Cardiology Billing
In 2026, cardiology billing errors often stem not from incorrect CPT selection, but from modifier misuse, E/M complexity underreporting, and incomplete linkage between diagnoses and services. Claims that lack clarity are increasingly downcoded or partially paid without triggering immediate alerts.
Over time, these underpayments accumulate into significant revenue leakage. Practices that do not routinely analyze remittance data and reimbursement trends may never realize how much revenue is being lost. A proactive cardiology billing strategy must include regular audits, denial trend analysis, and ongoing education for both providers and billing staff.
Orthopedic Billing After the 2026 Medicare Physician Fee Schedule
Global Surgical Package Enforcement Intensifies
Orthopedic practices are particularly impacted by CMS’s strict interpretation of global surgical packages under the 2026 PFS. Medicare continues to narrow what it considers separately billable during pre- and post-operative periods, placing greater responsibility on practices to justify exceptions.
Post-operative visits, complication management, and additional procedures must be carefully documented and billed according to Medicare rules. Claims submitted without clear differentiation between bundled and non-bundled services are increasingly denied or recouped during audits.
For orthopedic practices, billing accuracy begins in the operating room. Surgeons and clinical staff must document procedures and follow-up care with billing requirements in mind. Without this alignment, even high-performing practices risk systematic underbilling or repeated denials.
Implant and Supply Billing Under Reimbursement Pressure
Implant costs continue to rise, while Medicare reimbursement remains constrained. In this environment, orthopedic practices cannot afford missed charges, delayed billing, or incomplete documentation related to implants and supplies.
Billing teams must ensure that implant usage is thoroughly documented, appropriately coded, and submitted in a timely manner. Any breakdown in this process directly impacts reimbursement and can turn complex surgical cases into financial losses.
Radiology Billing After the 2026 Medicare Physician Fee Schedule
Continued Pressure on Imaging Reimbursement
Radiology practices have faced sustained reimbursement pressure for years, and the 2026 PFS reinforces this trend. CMS continues to adjust payments based on assumptions that imaging technology has reduced costs and increased efficiency.
In reality, radiology practices are investing heavily in equipment upgrades, cybersecurity, compliance infrastructure, and specialized personnel. These investments are necessary to meet regulatory requirements and maintain diagnostic accuracy, yet reimbursement does not reflect these costs.
Billing precision is therefore critical. Radiology claims must be submitted with complete documentation, correct component reporting, and accurate modifier usage to avoid delays and denials.
Authorization and Workflow Challenges in Radiology Billing
Radiology billing issues often originate upstream, before services are even rendered. Authorization failures, eligibility errors, and incomplete orders are among the most common causes of denied imaging claims.
Without integrated workflows between scheduling, clinical, and billing teams, these issues are difficult to catch in time. In 2026, radiology practices that fail to address front-end processes are seeing increased AR days and cash-flow disruptions.
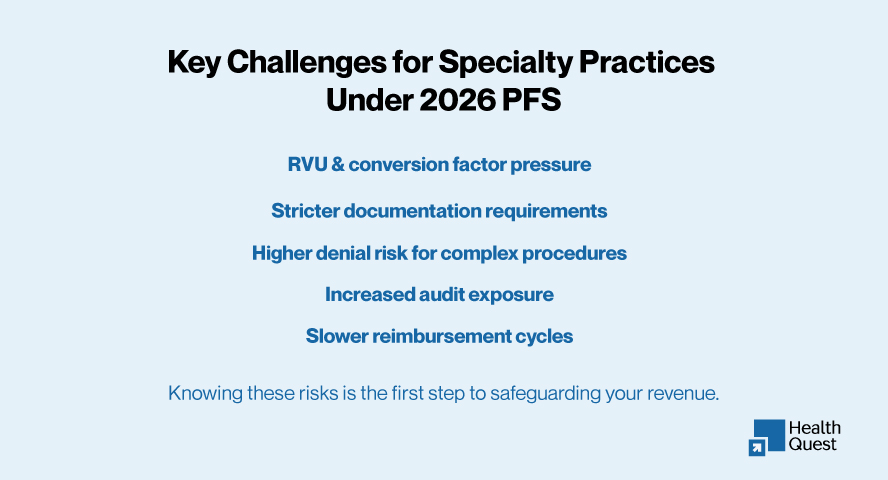
Shared Financial and Compliance Risks Across Specialty Practices
Rising Denial Rates and Audit Exposure
Across cardiology, orthopedics, and radiology, denial rates are rising due to stricter payer interpretations and heightened audit activity. Medicare and Medicare Advantage plans are increasingly targeting high-cost services for review, placing specialty practices under greater compliance pressure.
Audits are no longer limited to large health systems. Independent and mid-sized specialty practices are equally at risk, particularly when documentation and coding practices are inconsistent or outdated.
Cash-Flow Instability in a Low-Margin Environment
Delayed reimbursements and underpayments directly affect a practice’s ability to manage payroll, vendor relationships, and operational planning. In 2026, cash-flow instability is often a symptom of billing inefficiencies rather than patient volume issues.
Practices that lack visibility into their AR performance, denial trends, and payer behavior struggle to respond quickly. This reactive approach increases financial risk and administrative burden.
Shared Financial and Compliance Risks Across Specialty Practices in 2026
The 2026 Medicare Physician Fee Schedule introduces consistent financial and compliance risks across procedural specialties. Tighter reimbursement models, stricter documentation requirements, and higher denial sensitivity mean even small billing gaps now result in measurable revenue loss. These issues rarely appear all at once; they accumulate quietly through underpayments, delayed claims, and avoidable denials.
| Specialty | Primary Risk | Estimated Annual Revenue Impact | Common Billing Exposure |
| Cardiology | RVU compression and downcoded or denied E/M services | $30,000–$75,000 | Missed E/M complexity, underreported follow-ups, echocardiograms downcoded due to weak documentation |
| Orthopedics | Global period misreporting and implant billing errors | $45,000–$120,000 | Unbilled post-op services, implant charges denied or reduced due to incomplete operative notes |
| Radiology | Technical component cuts and authorization failures | $35,000–$90,000 | MRI/CT denials caused by missing authorizations or incorrect component billing |
| Multi-Specialty / Multi-State Practices | Fragmented workflows and payer rule variability | $100,000+ | Missed charges, delayed payments, and compliance gaps across locations and payers |
In 2026, protecting specialty revenue requires proactive billing oversight, consistent documentation standards, and payer-specific validation. Without these controls, reimbursement pressure quickly turns into sustained cash-flow instability.
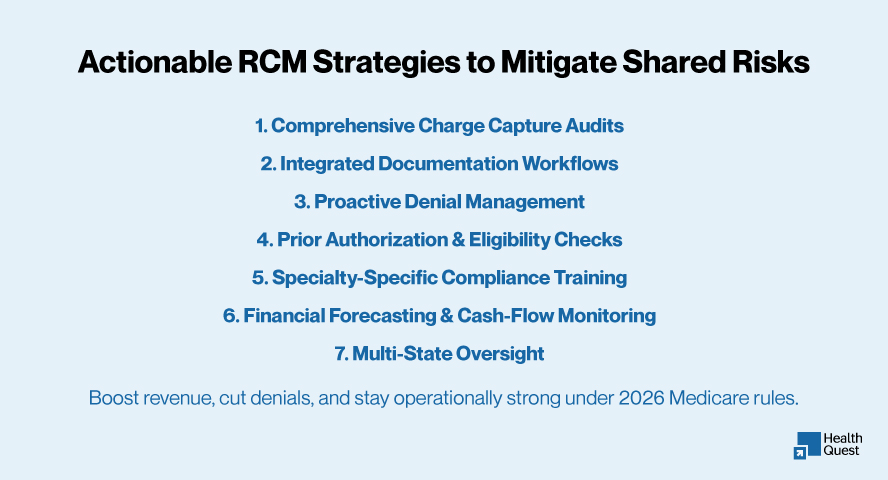
Building a Resilient Billing Strategy for 2026 and Beyond
To protect revenue under the 2026 Medicare PFS, specialty practices should adopt a proactive and data-driven revenue cycle management approach:
Shifting From Reactive to Preventive Revenue Cycle Management
The most successful specialty practices in 2026 are those that have shifted from reactive billing to preventive revenue cycle management. This approach focuses on getting claims right the first time rather than relying on appeals to recover lost revenue.
Preventive strategies include charge capture audits, documentation alignment, payer-specific coding updates, and continuous performance monitoring. These efforts reduce denial rates, shorten AR cycles, and stabilize cash flow.
The Role of Data and Analytics in Protecting Revenue
Data-driven decision-making is no longer optional. Practices must analyze denial patterns, reimbursement trends, and payer behavior to identify vulnerabilities in their revenue cycle.
By using data to anticipate issues rather than respond to them, specialty practices can adapt quickly to policy changes and payer tactics introduced under the 2026 PFS.
How Health Quest Billing Helps Specialty Practices Thrive Under the 2026 Medicare PFS
Health Quest Billing delivers comprehensive, Medicare-focused revenue cycle management designed for cardiology, orthopedics, radiology, and other procedural specialties. Our services are tailored to help practices navigate the complexities of the 2026 PFS while maximizing revenue and minimizing compliance risk.
We partner with practices to:
- Anticipate reimbursement changes by analyzing CMS updates and projecting financial impact across key CPT codes.
- Optimize coding and documentation to ensure every service E/M visits, diagnostic procedures, imaging, surgeries, and post-operative care is accurately captured and compliant.
- Prevent denials before they happen with proactive claim scrubbing, payer-specific validations, and real-time authorization tracking.
- Recover revenue efficiently through automated denial management, root-cause analysis, and targeted appeal strategies.
For multi-state or multi-specialty practices, we monitor local coverage determinations, Medicare Advantage rules, and evolving CMS guidance to ensure consistent billing, faster reimbursements, and minimal disruptions, no matter where services are delivered.
By aligning clinical workflows with Medicare requirements, Health Quest Billing reduces administrative burden, strengthens compliance, and ensures practices maintain healthy cash flow, even under the tighter 2026 PFS rules.
Final Thoughts:
The 2026 Medicare Physician Fee Schedule makes one reality clear specialty billing success is no longer driven by volume alone. Cardiology, orthopedics, and radiology practices must treat billing accuracy, documentation quality, and revenue cycle strategy as core business functions.
Practices that adapt now will be better positioned to withstand ongoing reimbursement pressure and regulatory scrutiny. Those who delay risk compounding revenue loss in an environment where margins leave no room for error. In 2026 and beyond, precision, not volume, defines financial stability in specialty billing.
Partners with Medicare billing review with Health Quest Billing today to navigate these challenges with confidence, protecting revenue, reducing denials, and ensuring billing operations are built for 2026 and beyond.