The demand for outpatient surgical care is rising, and ASC credentialing is more critical than ever as surgical volumes are projected to grow by 18% by 2033. Better credentialing is essential to ensure compliance and patient safety. This process verifies provider qualifications, including NPI, state licenses, DEA registration, and board certifications. Credentialing maintains trust, supports operations, and meets regulatory standards for ASC accreditation and Medicare certification.
In this blog, we will break down the essential steps of Ambulatory Surgical Centers’ credentialing, including provider verification, regulatory compliance, and accreditation requirements. You’ll gain insights into how credentialing ensures patient safety, maintains operational stability, and meets industry standards for Medicare and state licensure.
Credentialing for Ambulatory Surgical Centers (ASC)
In healthcare, ASC credentialing is the process of verifying the educational background, licenses, certifications, and professional history of healthcare providers to ensure that the providers meet the standards of the industry, state, and federal policies. In this process, the following documents are verified:
- Medical licenses
- Board certifications
- Malpractice history
- Liability insurance
- Compliance with Medicare & others
ASC credentialing helps maintain patient safety, regulatory compliance, and the overall quality of care in ASC.
Why is credentialing important for ASC?
Ambulatory Surgical Centers credentialing is not just a regulatory requirement; it is the foundation of patient safety, trust, and efficient ASC operations. With nearly 10,000 ASC operating in the U.S, ensuring that healthcare providers are thoroughly vetted is crucial.
Here’s why ASC’s credentialing is essential:
- Enhancing Patient Safety: Proper credentialing ensures that only trained and certified providers treat patients, reducing the risk of complications and medical errors.
- Protecting the ASC’s Reputation: A well-credentialed team builds confidence among patients, insurers, and regulatory bodies, reinforcing the ASC’s commitment to quality care.
- Reducing Liability Risks: Verifying provider credentials helps shield ASC from potential legal issues related to malpractice or negligence.
- Ensuring Insurance Reimbursement: Most insurers require credentialing proof for reimbursement, making it critical for financial sustainability.
Key Steps in Credentialing Services for Ambulatory Surgical Centers
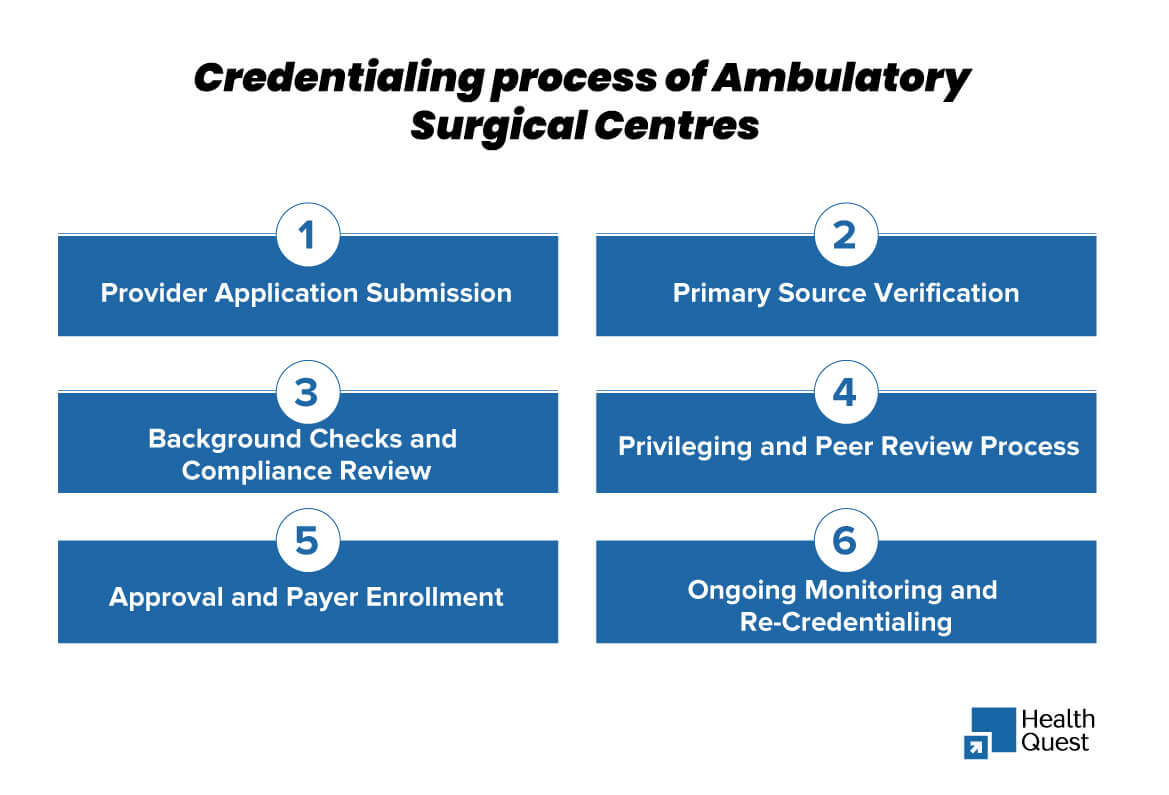
ASC credentialing process is crucial as it is designed to verify the provider’s qualifications, ensure compliance with regulatory standards, and maintain high-quality patient care. Below are the specific steps involved in ASC credentialing:
1. Provider Application Submission
The Ambulatory Surgical Centers credentialing process begins with healthcare providers submitting a detailed application, which includes:
- Medical licenses and board certifications
- Educational background and training records
- Hospital affiliations and work history
- Malpractice insurance coverage
- Professional references
- National Provider Identifier (NPI) number
2. Primary Source Verification
ASC must verify the accuracy of the submitted documents by directly contacting:
- Medical licensing boards
- Certification organizations (e.g., American Board of Medical Specialties)
- Previous employers and hospital affiliations
- The Drug Enforcement Administration (DEA) for controlled substance registration
3. Background Checks and Compliance Review
To mitigate risks, ASC conduct thorough background checks, which include:
- Malpractice history and any prior legal claims
- Medicare and Medicaid exclusions (checking databases like the OIG Exclusion List and the NPDB)
- Any disciplinary actions by medical boards or licensing authorities
This step helps ensure that ASCs are not employing providers with a history of fraud, abuse, or other violations.
4. Privileging and Peer Review Process
Once verification is complete, the ASC’s credentialing committee reviews the provider’s qualifications and determines their specific clinical privileges. This involves:
- Assessing the provider’s experience in performing outpatient procedures
- Matching skill sets with the ASC’s scope of services
- Consulting with specialty-specific peer reviewers if needed
The committee grants privileges only for procedures the provider is fully trained and competent to perform in an outpatient setting.
5. Approval and Payer Enrollment
After credentialing and privileging, the provider is officially approved to practice at the ASC. This step includes:
- Enrolling the provider with Medicare, Medicaid, and commercial insurance companies
- Ensuring proper documentation for reimbursement and billing compliance
- Registering with Managed Care Organizations (MCOs), if applicable
Without proper enrollment, Ambulatory Surgical Centers face credentialing risk, claim denials, and payment delays.
6. Ongoing Monitoring and Re-Credentialing
Medical credentialing is not a one-time process. ASCs must continuously monitor provider qualifications and renew credentials periodically, typically every two to three years. This includes:
- Verifying renewed medical licenses, DEA registrations, and insurance coverage
- Reviewing updated malpractice history and any new disciplinary actions
- Conducting periodic peer reviews and quality assessments
Common Challenges in Credentialing for Ambulatory Surgical Centers (ASCs)
ASC’s credentialing is a detailed and time-sensitive process. While it ensures compliance and patient safety. This aims to ensure compliance and patient safety, it also comes with several challenges that can delay operations and impact financial stability. Here are some of the hurdles ASCs face during credentialing.
Lengthy and Complex Verification Process
Credentialing timelines can vary widely, but they typically range from 60 to 120 days, depending on factors such as the provider’s background and the responsiveness of primary sources like licensing boards. Due to complications, the process sometimes goes beyond 180 days.
Frequent Changes in Regulatory Requirements
ASCs must comply with evolving regulations from organizations such as Medicare, the Joint Commission (TJC), and the Accreditation Association for Ambulatory Health Care (AAAHC). Keeping up with these changes and ensuring compliance can be challenging, especially for smaller ASCs with limited administrative resources.
Insurance and Payer Enrollment Delays
Even after a provider is credentialed, payers such as Medicare, Medicaid, and private insurers may take months to approve enrollment. This delay affects the ASC’s ability to bill for services, leading to potential revenue losses.
Re-Credentialing and Ongoing Compliance
ASCs credentialing is not a one-time process. ASCs must track expiration dates for medical licenses, DEA registrations, malpractice insurance, and board certifications. Missing a re-credentialing deadline can result in a provider losing privileges, affecting patient care and revenue flow.
Inconsistent Documentation from Providers
Many credentialing delays stem from incomplete or inaccurate provider applications. Missing documents, outdated references, or incorrect information require additional follow-ups, slowing down the approval process.
High Administrative Burden
Credentialing is a resource-intensive process, requiring dedicated staff to handle paperwork, verifications, and communication with various agencies. ASCs with limited administrative teams may struggle to keep up with credentialing demands.
Risk of Compliance Violations
Failing to properly credential or re-credential providers can lead to compliance violations, legal penalties, and even the loss of accreditation. Regulatory bodies and insurance payers conduct audits, and any gaps in documentation can result in fines or service restrictions.
Credentialing Software and Data Management Issues
Many ASCs still rely on manual processes or outdated software for credentialing, leading to inefficiencies and errors. Without a centralized credentialing system, tracking provider data, renewal deadlines, and compliance requirements becomes difficult.
How Professional Credentialing Services Can Help ASCs
Credentialing for Ambulatory Surgical Centers (ASCs) is a complex process that can lead to delays, compliance risks, and administrative burdens. Professional credentialing services simplify this process, ensuring efficiency, accuracy, and regulatory compliance.
Key Benefits of Professional Credentialing Services
Image title: Benefits of professional credentialing services
- Faster Verification: Direct coordination with licensing boards and automated tracking reduces credentialing delays.
- Regulatory Compliance: Experts stay updated on Medicare, The Joint Commission (TJC), and AAAHC requirements, ensuring ASCs meet industry standards.
- Quicker Payer Enrollment: Credentialing specialists handle insurance approvals, minimizing reimbursement delays and revenue losses.
- Better Re-Credentialing: Services track expiration dates and manage renewals, preventing lapses in provider privileges.
- Error-Free Documentation: Professionals assist with application accuracy, reducing rejections and approval setbacks.
- Lower Administrative Burden: Outsourcing frees up ASC staff to focus on patient care and operations.
- Reduced Compliance Risks: Thorough background checks prevent legal issues and protect the ASC’s reputation.
- Advanced Software Integration – Many services use automated credentialing systems for efficient document management and tracking.
State-by-State Variations in Ambulatory Surgical Center (ASC) Credentialing
State-to-state variations in ASC credentialing are influenced by licensing requirements, Medicaid enrollment, payer policies, and accreditation standards. Here are the key differences:
State Licensing Requirements
- Each state has its own Medical Board or Health Department overseeing ASC credentialing.
- Some states, like California and Texas, have stricter regulations on facility accreditation and provider licensing.
- New York requires additional approvals from the Public Health and Health Planning Council for ASCs.
Medicaid Enrollment & Reimbursement
- Medicaid credentialing rules vary; Florida and Texas have separate managed care enrollment requirements.
- California’s Medi-Cal may take longer for provider enrollment compared to states with streamlined processes.
Commercial Payer Contracts
- Private insurers have state-specific credentialing policies; Blue Cross Blue Shield of Texas may have different enrollment timelines than BCBS of Illinois.
- Some states have mandated timelines for payer credentialing, while others leave it to insurers’ discretion.
Accreditation & Compliance Standards
- States like New Jersey require ASCs to obtain licensure before accreditation from organizations like AAAHC or TJC.
- Some states mandate additional infection control measures, such as New York’s heightened surgical facility regulations.
Re-Credentialing & Ongoing Compliance
- California and Massachusetts have stricter re-credentialing cycles, often requiring updates every two years.
- States like Florida impose penalties for lapses in credentialing, impacting ASC operations.
- ASC must track renewal dates for medical licenses, DEA registrations, and board certifications. Using CAQH ProView simplifies the process.
Final Thoughts
Credentialing is the backbone of a well-functioning Ambulatory Surgical Center, ensuring compliance, patient safety, and financial stability. While the process can be time-consuming and complex, professional credentialing services help streamline approvals, reduce administrative burdens, and prevent costly delays.
By investing in a reliable credentialing solution, ASC can focus on what truly matters, delivering high-quality outpatient surgical care with confidence and efficiency. Partnering with experts like Health Quest ensures that your ASC remains compliant, operationally sound, and financially secure in an ever-evolving healthcare landscape.
Why Partnering with a Credentialing Service, Health Quest is a Smart Choice
By outsourcing credentialing to experts like Health Quest, ASC can improve efficiency, maintain compliance, and ensure timely provider approvals. This not only enhances patient safety and operational stability but also supports financial growth by preventing credentialing-related revenue losses.
Contact us today at: (415) 508-653. Let us take the stress out of credentialing for you!