Patient education is a core part of physical therapy 99% of PTs consider it essential, and it can reduce care costs by 29% while boosting satisfaction by 33%.
The challenge? Billing for it. Many PTs are unsure which CPT codes apply, how Medicare’s 8-Minute Rule works, or if insurers even cover it.
This guide explains all the codes, rules, documentation and common mistakes so you can bill correctly and get paid for the time you spend teaching.
Why Is Patient Education Important in Physical Therapy
Patient education isn’t just about giving instructions; it’s about empowering people to take charge of their recovery. When therapists spend time teaching patients the “why” and “how” behind their care, the results go far beyond the clinic:
- Patients are more likely to stick to their home exercise programs.
- They’re at a lower risk of reinjury or hospital readmission.
- Chronic conditions become easier to manage on a day-to-day basis.
- Overall recovery is faster and more effective.
But while the clinical impact is clear, billing for patient education is not always simple. Many practices struggle to align documentation with payer rules, especially when education blends into therapeutic activity. To ensure accurate reimbursement, providers must understand which CPT codes apply, how Medicare’s 8-minute rule works and how to document skilled instruction properly, often where PT billing services become essential for accuracy and compliance.
Can Physical Therapists Bill for Patient Education?
The answer is yes, but only under certain conditions. Here’s how it works:
- When it is billable: Education that requires professional skill and is directly tied to the therapy plan.
Example: Teaching a patient the correct way to perform therapeutic exercises at home.
- When it is not billable: General advice or unsupervised instruction that does not require the expertise of a therapist.
Example: Handing out a printed exercise guide without demonstration or skilled input.
- How to bill it:
- Document the education as part of a time-based CPT code, such as therapeutic exercise (97110) or neuromuscular re-education (97112).
- Use specific codes like 98960–98962 only if you are providing a structured self-management education program.
- Document the education as part of a time-based CPT code, such as therapeutic exercise (97110) or neuromuscular re-education (97112).
How to Bill Patient Education in Physical Therapy (PTs)
Patient education plays a huge role in outcomes, but billing for it often feels like walking a fine line. Therapists know the value of teaching, whether it’s explaining safe movement techniques, coaching through a home exercise program, or showing a caregiver how to assist. Still, payers don’t always make it simple. The key is to understand which CPT codes apply, when they apply, and how to document them so that education is recognized as a billable service.
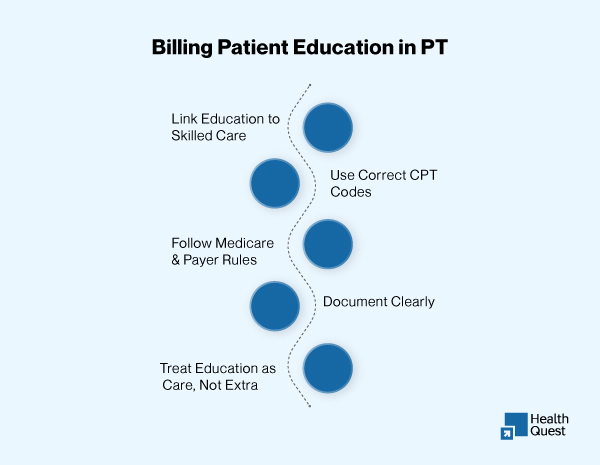
Connect Education to Skilled Therapy Services
Insurance companies (including Medicare) will not reimburse for “casual” education. Simply handing out a pamphlet or having a quick chat about posture isn’t enough. To be billable, the education must require your professional expertise and be tied directly to the therapy plan.
- Teaching a patient correct form for therapeutic exercises → 97110
- Guiding a patient through balance or motor control retraining → 97112
- Educating on safe functional movements (lifting, walking, transfers) → 97530
Use Specialized CPT Codes When Applicable
Some educational activities go beyond exercise instruction and fall under codes designed for education:
- 98960–98962: Self-management education, used when delivering a structured, evidence-based curriculum (often for chronic disease management). Sessions must be 30 minutes each, face-to-face, and may include caregivers.
- 97550–97552: Caregiver training, used when educating caregivers only (without the patient present). Medicare reimburses these codes as long as training is part of a therapy plan of care.
Follow Medicare and Payer-Specific Rules
Billing isn’t just about choosing a CPT code; payer rules can change the outcome.
- Medicare 8-Minute Rule: For time-based therapy codes (97110, 97112, 97530), education time is billable only if it meets the 8-minute minimum and is documented as skilled instruction.
- Commercial payers: Some will reimburse self-management codes like 98960, while others may deny them. Policies differ widely.
- Medicaid programs: Rules vary by state, so check your local guidelines.
Document Clearly and Defensibly
Education-related billing succeeds or fails based on documentation. You must show what you taught, how much time you spent, and why it required skilled input. Strong documentation includes:
- Time spent: “12 minutes of instruction on therapeutic exercise techniques.”
- Content taught: “Educated patient on three HEP exercises: squats, bridges, clamshells.”
- Patient response: “Patient return-demonstrated with moderate corrections.”
- Clinical reasoning: “Skilled instruction was required to ensure proper form and prevent knee strain.”
Think of Education as Part of the Treatment, Not Extra
The best way to approach billing is to stop treating education as an “add-on.” Instead, think of it as integrated into the therapy session. When you’re teaching, you’re not just talking, you’re applying your professional expertise to ensure the patient learns movements correctly, understands precautions, and can safely carry out their plan of care. That is skilled therapy, and it deserves to be billed as such.
Billing Patient Self-Management Education Codes
Physical therapists can sometimes bill self-management education codes (98960–98962) when providing a structured program for patients managing chronic conditions such as arthritis, COPD, or asthma. These codes apply only when:
-
A physician orders the program
-
A licensed non-physician provider delivers it
-
A standardized, evidence-based curriculum is used with measurable outcomes
Code use:
-
98960 – Individual patient (30 minutes)
-
98961 – 2–4 patients
-
98962 – 5–8 patients
Important: Medicare does not reimburse these codes, and many private payers follow the same policy. Always confirm payer coverage before billing.
Common billing mistakes in physical therapy:
Billing for patient education in physical therapy can feel tricky, and it’s easy to make mistakes that cost you time, money, and even trigger compliance concerns. Here are the most common pitfalls and how to avoid them.
Overusing Non-Billable Codes
One of the biggest causes of physical therapy overbilling is trying to use non-billable codes for education that don’t meet the requirements. For example, simply giving a patient a handout or having a casual conversation about posture is not considered skilled therapy. If you try to bill for that time, you run the risk of denials or worse, being flagged for PT billing errors.
Documenting Too Vaguely
Writing “patient educated” in your notes isn’t enough. Vague documentation is one of the fastest ways to lose reimbursement during an audit. If your documentation doesn’t clearly show what you taught, how long you spent, and why it required professional expertise, payers won’t recognize it as billable.
Forgetting to Link Education to Functional Goals
Education in physical therapy is only billable when it’s connected to a patient’s functional outcomes. If you don’t clearly show that connection, payers may treat it as non-billable advice.
Assuming Payers Cover CPT 98960 Without Checking
The CPT 98960 series is designed for structured self-management education, but not every insurer reimburses it. Some commercial payers cover it, while others deny it outright. Assuming it’s universally covered can lead to repeated denials and frustration.
Medicare vs. Commercial Payers vs. Medicaid: Who Covers Patient Education?
Billing for patient education isn’t one-size-fits-all. Coverage depends on the payer, and the rules can vary significantly between Medicare, commercial insurers, and Medicaid. Below is a breakdown of how each handles it.
| Payer | How It’s Billed | Codes Covered | Key Rules |
| Medicare | Only billable when part of skilled, time-based therapy (97110, 97112, 97530). | Does not cover 98960–98962. Allows caregiver codes 97550–97552. | Must follow the 8-Minute Rule. Documentation must show skilled instruction tied to goals. |
| Commercial | More flexible; some plans reimburse for structured self-management education. | May cover 98960–98962, plus standard PT codes (97110, 97112, 97530). | Coverage varies by plan and always checks payer policy. |
| Medicaid | State-specific. Most cover education under skilled therapy codes. | Some states allow 98960–98962, many don’t. Caregiver codes are often accepted. | Check the state Medicaid manual for rules. |
Denials and Appeals for Patient Education Billing
Even when billed correctly, patient education can get denied. Here’s what to know:
Common Denial Reasons
- Vague documentation: Notes like “patient educated” without details.
- Lack of medical necessity: Education not linked to therapy goals.
- Unsupported CPT code: Using 98960–98962 when the payer doesn’t cover it.
How to Appeal
- Submit clear documentation showing time, content, patient response, and clinical reasoning.
- Reference the patient’s therapy plan and functional goals.
- Include payer-specific rules that justify the service.
CPT 98960 for Physical Therapy
CPT 98960 is defined as “Education and training for patient self-management by a qualified, non-physician healthcare professional, face-to-face with the patient, 30 minutes, individual.”
In physical therapy, this code is used when a PT provides a structured, evidence-based self-management education program. It’s most often applied for chronic conditions such as diabetes, arthritis, or chronic pain, where patient training plays a direct role in long-term management.
Key Points to Know:
- Time requirement: Must be at least 30 minutes face-to-face.
- Format: Can be billed for one patient (98960), 2–4 patients (98961), or 5–8 patients (98962).
- When appropriate: Only when delivering a structured program that goes beyond basic exercise instruction.
- Limitations: Medicare generally does not reimburse 98960–98962, but some commercial insurers and Medicaid programs may cover them. Always check payer policies before billing.
- Documentation: Clearly outline the program provided, patient participation, and the clinical need for education.
Example in PT Practice:
“A therapist runs a chronic low back pain management program where patients learn pacing, safe lifting strategies, posture correction, and self-monitoring techniques. Each session is 30 minutes, face-to-face, with structured goals and measurable outcomes. This may qualify under CPT 98960”.
How to Document Patient Education Correctly
When billing for patient education, your notes must show more than “patient educated.” Use this checklist to make sure you cover all the essentials:
- Time spent: Record exact minutes (follow the 8-Minute Rule or 30-min requirement for 98960).
- Content taught: List specific exercises, strategies, or topics covered.
- Patient response: Document return demonstration, understanding, or questions asked.
- Skilled input: Explain why a therapist’s expertise was required (e.g., to correct form, prevent injury).
- Connection to goals: Link education to functional or therapy plan goals.
- Caregiver involvement (if applicable): Note when caregiver training was provided.
Final Thoughts
Patient education is essential in physical therapy; it improves outcomes and keeps patients engaged. To get reimbursed, link education to skilled therapy, use the right CPT codes, follow payer rules, and document clearly.
Treat education as part of care, not an add-on, and you’ll protect your practice, get paid for your expertise, and help patients recover safely and effectively.
Struggling with Patient Education Billing?
Getting reimbursed for patient education can be confusing, with unclear CPT codes, payer rules, and documentation requirements. At Health Quest, we help physical therapists deal with these challenges, reduce denials, and ensure every minute of skilled education is properly billed.
Schedule an appointment with our billing experts to improve your PT billing and get paid for the care you provide.