Starting a new role or launching your internal medicine practice? Before you see patients, you need to be credentialed.
In 2025, about 92% of Americans have health insurance, making credentialing essential for getting reimbursed. Most insurers, including Medicare, won’t accept claims unless you’re properly credentialed.
For internal medicine providers, credentialing ensures you can bill payers, stay compliant, and avoid costly delays. This guide walks you through the process step by step, so you can get credentialed faster and start seeing patients sooner.
What is Medical Credentialing for Internal Medicine?
Medical credentialing is the process of verifying a provider’s qualifications, like medical school, residency, board certification, licenses, and work history. For internal medicine physicians, this step is crucial before joining insurance networks or treating patients in hospitals.
Why is it especially important in internal medicine? Internists handle a wide range of adult health issues, often managing chronic conditions and coordinating complex care. Because of this broad scope and high patient volume, payers and hospitals require thorough credentialing to ensure safe, qualified care.
Credentialing allows you to:
- Join insurance networks (Medicare, Medicaid, commercial plans)
- Bill payers are legally entitled to get reimbursed
- Obtain hospital privileges
- Stay compliant with healthcare regulations
Step-by-Step Credentialing Process for Internal Medicine Physicians
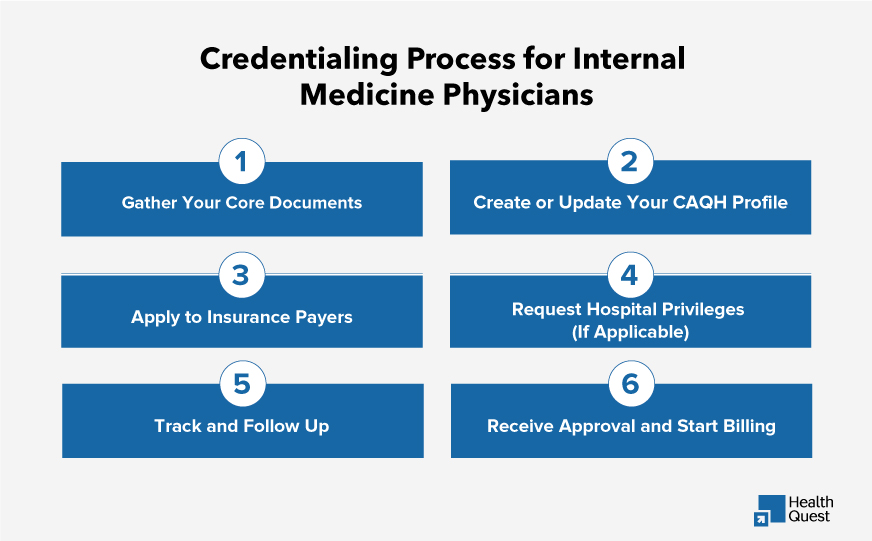
Credentialing can feel like a lot of paperwork, but when done right, it keeps your practice running smoothly. Here’s how the process typically works:
Gather Your Core Documents
Start by collecting essential credentials, which are essential for you to get easily credentialed:
- State medical license
- DEA certificate
- Board certification (ABIM or equivalent)
- Malpractice insurance details
- NPI (National Provider Identifier)
- Up-to-date CV with work history and references
Having these ready helps speed up the entire process.
Create or Update Your CAQH Profile
Most commercial payers use CAQH ProView to verify your information. Make sure your profile is complete, accurate, and attested (digitally confirmed) every 120 days.
Apply to Insurance Payers
Submit credentialing applications to Medicare, Medicaid, and private insurers (like Aetna, BCBS, Cigna, etc.). Each has different requirements, so attention to detail matters.
Request Hospital Privileges (If Applicable)
If you’ll admit or manage inpatients, you’ll need to apply for privileges at each facility. This process often includes peer references and committee reviews.
Track and Follow Up
Credentialing can take 90–120 days, sometimes longer. Regular follow-ups help prevent delays caused by missing documents or stalled applications.
Receive Approval and Start Billing
Once approved, you’ll receive notification, effective dates, and payer IDs, and then you’re cleared to start billing.
Credentialing Challenges Unique to Internal Medicine Physicians
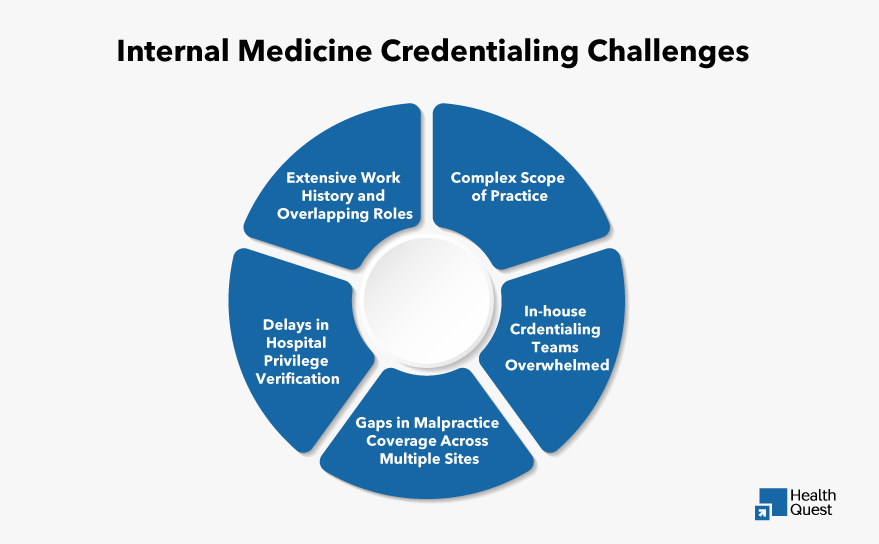
During Internal Medicine Credentialing, providers face unique hurdles due to their broad scope of services and high patient volume. Here are the most common issues that slow the process and how to stay ahead of them:
Extensive Work History and Overlapping Roles
Internists often work in hospitals, clinics, and outpatient settings, sometimes all at once. Listing multiple overlapping roles or part-time assignments without clear start/end dates can raise red flags for payers.
Complex Scope of Practice
Internal medicine covers a wide range of diagnoses and treatments, which sometimes confuses credentialing departments about what services you’re authorized to provide.
Delays in Hospital Privilege Verification
Since many internists hold hospital privileges, verification can be slow, especially if the hospital’s medical staff office is backlogged.
Gaps in Malpractice Coverage Across Multiple Sites
Dealing with multiple facilities can increase the risk of lapses or unclear coverage periods in malpractice insurance.
In-house Credentialing Teams Overwhelmed
In group practices, internal credentialing teams may be stretched thin, leading to inconsistent follow-ups and missed payer deadlines.
Credentialing Timeline and Cost Expectations for Internal Medicine Providers
Credentialing isn’t a quick process, and for internal medicine physicians, the timeline can vary depending on your scope of work and where you’re applying.
On average, initial credentialing takes 90 to 120 days, but delays are common if you’re applying to multiple commercial payers or hospital networks. Medicare and Medicaid enrollment can move faster (60–90 days), but private insurers often require more back-and-forth, especially if you work across several sites or hold hospital privileges.
Group practices with centralized credentialing teams may be able to improve some of the paperwork, but solo interns or those joining smaller practices often face longer timelines due to limited admin support.
As for costs, while there’s typically no direct fee for credentialing with payers, you may incur costs for:
- Application services or consultants: $200–$500 per payer, if outsourced
- Hospital privileging fees: Some facilities charge $100–$300 per application
- Credentialing software or CAQH management tools (optional): Variable pricing
- Lost revenue from delays: This is often the biggest hidden cost. If you’re not credentialed, you can’t bill
Don’t Forget Re-Credentialing
Credentialing isn’t a “set it and forget it” process. Most payers require re-credentialing every 2 to 3 years to maintain active participation in their networks. This means you’ll need to resubmit or update documentation like your license, board certification, work history, and malpractice insurance.
CAQH Attestation Reminder:
If you’re using CAQH ProView (as most internists do), you must attest your profile every 120 days, even if nothing has changed. Failure to do so can flag your profile as inactive and delay payer approvals.
What happens if you miss re-credentialing?
- Claims may be denied or pending.
- You could be terminated from insurance panels without notice.
- Reinstatement can take weeks or months, resulting in lost revenue
State-Specific Credentialing Rules
Keep in mind: Credentialing requirements can vary by state, especially for Medicaid enrollment, hospital privileges, and background checks. Some states may require additional forms, W-9s, or fingerprinting. If you’re practicing in multiple states, be sure to check each one’s process separately to avoid delays.
In-House vs. Outsourced Credentialing: What’s Best for Internal Medicine Providers?
Credentialing is time-sensitive and complex, especially for internal medicine doctors managing multiple payers, hospital privileges, and a high volume of patients. How you manage it can make or break your reimbursement timeline.
In-House Credentialing
Some practices choose to handle credentialing internally using admin staff or office managers. While this may seem cost-effective, it often leads to delays and rework, especially without a dedicated credentialing expert.
- Admin staff are often overworked or lack credentialing experience
- Missed deadlines or outdated CAQH profiles cause application rejection
- Difficult to keep up with payer-specific requirements and hospital verifications
Outsourced Credentialing
Outsourcing lets you hand off the process to trained specialists who manage everything from start to finish. This can drastically reduce errors and speed up approval times.
Benefits of outsourcing:
- Faster processing and fewer delays
- Experts track deadlines, manage documents, and stay updated on policies
- Frees up internal staff to focus on patients, not paperwork
- Ideal for internists working across multiple locations or joining new payer networks
Why Internal Medicine Doctors Choose Our Credentialing Services?
Internal medicine Credentialing isn’t one-size-fits-all. With multiple payers, hospital affiliations, and compliance requirements, it takes experience to get it right and fast.
That’s where we come in.
We specialize in credentialing support for internists, offering:
- Medicare, Medicaid, and commercial payer enrollment
- CAQH profile setup and maintenance
- PECOS and Medicaid revalidation
- Hospital privilege applications
Final Thought
Credentialing may feel like a mountain of paperwork, but it’s one of the most important foundations of your internal medicine career. Whether you’re opening your practice, joining a group, or switching networks, getting credentialed the right way ensures you can see patients, get reimbursed, and grow without unnecessary setbacks.
With a trusted partner by your side, the process doesn’t have to be stressful or time-consuming. Let credentialing be the start of your success, not the delay.
Ready to get credentialed with confidence? Contact us today for expert support tailored to internal medicine providers.