Massachusetts healthcare providers face a steep challenge in improving their revenue cycle. Statewide claim denials averaged 11.8% in 2023, slightly under the national pace but still a major drain on revenue. Compounding the pressure, 73% of practices nationwide saw denials rise in the past few years, with 38% admitting that over 10% of their claims were rejected. Against this backdrop, selecting the best medical billing company in Massachusetts isn’t just smart, it’s essential.
The right partner not only trims denials and improves collections but also frees you to focus on what matters most: patient care.
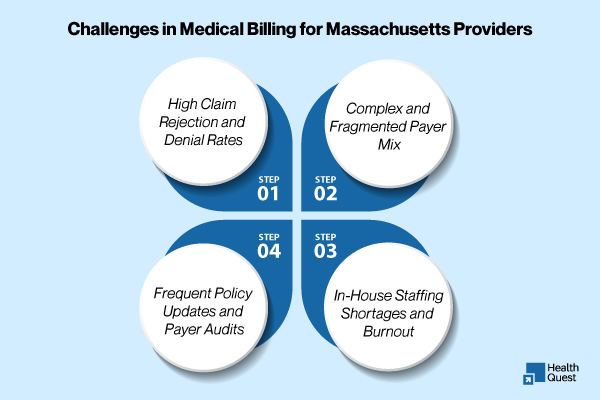
Why Massachusetts Providers Face Unique Billing Challenges
Massachusetts combines one of the nation’s most advanced health systems with a complex payer landscape. Key factors that make billing here uniquely challenging include:
-
MassHealth complexity. MassHealth’s policies and program updates, plus its role as a major payer, create frequent rule changes and special documentation requirements for Medicaid claims.
-
Diverse payer mix. Providers must manage claims for MassHealth, Medicare, Medicare Advantage, and multiple commercial insurers (Blue Cross Blue Shield of MA, Tufts, Harvard Pilgrim, etc.). Each payer has its own rules about modifiers, prior authorization, and timely filing.
-
Regulatory scrutiny and audits. Massachusetts payers and state auditors are active; incorrect submissions or provider enrollment errors can trigger lengthy appeals and audits.
-
Telehealth and evolving care models. Telehealth remains a significant and growing part of care delivery (for example, a meaningful share of Medicare beneficiaries used telehealth in 2024), requiring careful billing logic to match payer rules.
Because of these conditions, standard, off-the-shelf billing approaches often fail. Local expertise matters.
The Real Cost of Claim Denials
Denials eat into margins in multiple ways: lost revenue for unrecovered claims, higher AR days, extra staff time for appeals, and opportunity cost as clinicians and staff chase paperwork instead of patients. National and industry studies show that a significant portion of practices report a growing denial burden and many practices see more than 10% of claims rejected at least some of the time.
For Massachusetts providers, the hit can be amplified because re-submissions to MassHealth and major commercial payers often require extra documentation or manual intervention. On top of direct losses, prolonged AR increases working capital needs and creates cash-flow strain.
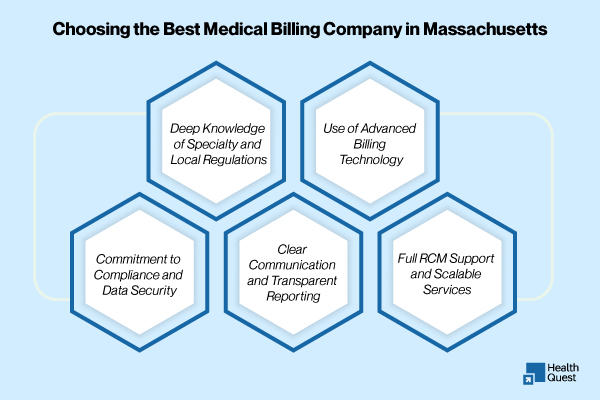
What Providers Should Look for in the Best Medical Billing Company in Massachusetts
When evaluating RCM partners, Massachusetts providers should prioritize capabilities that directly reduce denials and accelerate cash flow:
-
MassHealth & Local Payer Expertise — The partner must understand MassHealth nuances, MA payer-specific modifier and referral rules, and state filing deadlines.
-
Proactive Denial Prevention — Not just resubmitting denials, but preventing them with eligibility checks, front-end claim scrubbing, and training for front-desk staff.
-
Advanced Technology — AI claim scrubbing, integrated EHR/PM connectors, and dashboards that surface issues before claims leave your system.
-
Transparent Reporting — Clear KPIs: first-pass acceptance rate, denial reasons, days in AR, net collection rate.
-
Specialty Knowledge — Billing for behavioral health, pediatrics, cardiology, or orthopedics each has unique challenges — pick a partner with demonstrated specialty experience.
-
Credentialing & Enrollment Support — Correct provider enrollment prevents denials at the source.
Local Coverage Across Massachusetts
Health Quest Billing supports providers statewide, with experience across every setting — from major hospital networks to small private practices. We proudly serve:
-
Boston – academic medical centers, specialty clinics, and large hospital systems
-
Worcester – community health centers and multispecialty groups
-
Springfield – pediatric and behavioral health practices
-
Cambridge & Lowell – academic clinics and small group practices
-
Western MA & Cape Cod – rural providers and community-based clinics
Wherever your practice is located in Massachusetts, our team understands the local payer landscape and tailors solutions to your community’s needs.
Pricing Models & ROI — What to Expect in Massachusetts
Most billing firms use one of these models:
-
Percentage of collections (most common) — typically 4–8% depending on specialty, volume, and service scope.
-
Flat monthly fee — predictable for low-volume practices, but can be less flexible.
-
Hybrid — a small flat fee + reduced percentage on collections.
What matters more than the fee is net ROI.
Example: if a billing partner reduces denials by 30% and shortens days in AR, the practice often recovers multiples of the annual fee. A realistic ROI example: a 5-provider primary care practice that increases collections by 20–30% after optimized RCM can cover fees and add materially to net revenue.
Technology & Emerging Trends to Watch (2024–2025)
| Trend | What It Means | How Providers Benefit |
|---|---|---|
| AI Claim Scrubbing & Predictive Denial Analytics | AI tools flag high-risk claims before submission and help prioritize appeals. | Reduce denials, improve first-pass claim rate, and recover revenue faster. |
| Telehealth Billing Optimization | CMS and private payers continue updating telehealth coding and modifier rules. | Ensure accurate reimbursement for virtual visits and avoid compliance issues. |
| Value-Based Payment (VBP) Navigation | Includes bundled payments, quality reporting, and risk-based contracts. | Unlock new revenue streams by meeting quality metrics and payer incentives. |
| Increased Payer Audit Activity | Payers are ramping up chart reviews and compliance checks. | Strengthen documentation workflows, build audit-ready records, and reduce financial risk. |
| Consolidation in HealthTech & RCM | EHR and RCM platforms are merging and integrating more closely. | Streamlined workflows, fewer system silos, and more efficient billing operations. |
Top Reasons for Claim Denials in Massachusetts – With Solutions
| Denial Reason | Why It Happens | Solution |
|---|---|---|
| Eligibility Issues | Coverage expired, incorrect policy details, or ineligible services not caught before the visit. | Verify eligibility 72 hours before and again on the day of service using real-time payer portals or EDI tools. |
| Incomplete or Incorrect Documentation | Missing provider notes, referrals, prior authorizations, or required forms. MassHealth has particularly strict requirements. | Standardize documentation workflows, use EHR-integrated templates, and run internal audits to ensure completeness. |
| Coding Errors & Outdated Code Sets | Incorrect CPT, ICD-10, or modifier usage, especially after payer policy or annual code set updates. | Provide ongoing coder training, implement AI-assisted coding tools, and keep systems updated with the latest payer policies. |
| Untimely Filing | Claims or appeals submitted after payer deadlines due to internal processing delays. | Automate claim submission, set internal filing deadlines 5–7 days earlier than payer limits, and track with RCM dashboards. |
| Authorization & Referral Failures | Prior authorizations or referrals not obtained for specialty care, imaging, or surgeries. | Create authorization checklists, assign dedicated staff, and use payer portals for tracking and reminders. |
| Provider Credentialing or Enrollment Issues | Providers not properly enrolled or credentialed; mismatches in NPI or provider name data. | Regularly update credentialing files, monitor CAQH, and confirm active enrollment status with all payers. |
| Coordination of Benefits (COB) Confusion | Incorrect payer order for patients with dual coverage (e.g., Medicare + Medicaid). | Collect detailed insurance info at intake, confirm primary vs. secondary coverage, and update payer order in practice systems. |
How Health Quest Billing Solves These Problems (Local, Measurable Results)
Health Quest Billing combines local Massachusetts payer knowledge with modern RCM technology and white-glove client service. Key differentiators:
-
Local payer experience: Years working with MassHealth, BCBS MA, Tufts, and other major Massachusetts payers.
-
High clean-claim rates: We target and deliver clean-claim acceptance well above industry averages (client metrics often exceed 95% first-pass acceptance).
-
Denial reduction: Proven denial prevention strategies that typically lower rejections by 25–40% within the first 6–12 months.
-
Transparent KPIs & dashboards: Daily and weekly AR reporting so practice leadership can see cash flow progress in real time.
-
US-based support & dedicated account managers who understand local regulations and escalate payer issues on behalf of clients.
Final Thought:
In a state as fast-paced and highly regulated as Massachusetts, medical billing isn’t just a back-office function; it’s a strategic priority. Choosing the right billing partner can mean the difference between constant denials and consistent cash flow. With deep local expertise, smart technology, and a commitment to your success, Health Quest is here to help you take control of your revenue cycle so you can get back to focusing on patient care.
Health Quest Billing offers Massachusetts providers local payer expertise, advanced RCM tech, and a service model that delivers measurable results. If your practice is losing time and revenue to denials and slow AR, now is the time to act.
Get a free, no-obligation billing audit from Health Quest Billing and see how much revenue you’re currently leaving on the table. Contact us to schedule a 15-minute assessment and immediate recommendations.