Medical Billing in South San Francisco Is Changing Fast. As we move into 2026, healthcare providers in South San Francisco are facing a billing environment that is more demanding, more regulated, and less forgiving than ever before. Claim denials are rising, payer rules are tightening, reimbursement timelines are stretching, and medical coding requirements continue to evolve at a rapid pace. What worked even a year ago is no longer enough to protect your revenue.
For many practices, managing billing in-house has become a costly liability rather than a convenience. Staffing shortages, frequent payer updates, stricter audits, and growing patient financial responsibility are quietly draining revenue and increasing administrative burnout. Every delayed claim, missed modifier, or overlooked authorization now carries a higher financial risk.
In 2026, outsourcing medical billing is no longer just about saving time, it’s about safeguarding cash flow, maintaining compliance, and staying competitive in California’s complex healthcare landscape. This blog explores how professional medical billing services in South San Francisco help practices increase claim approval rates, stabilize revenue, reduce denials, and refocus their energy on what truly matters: delivering exceptional patient care without financial uncertainty.
Billing Challenges for South San Francisco Healthcare Providers
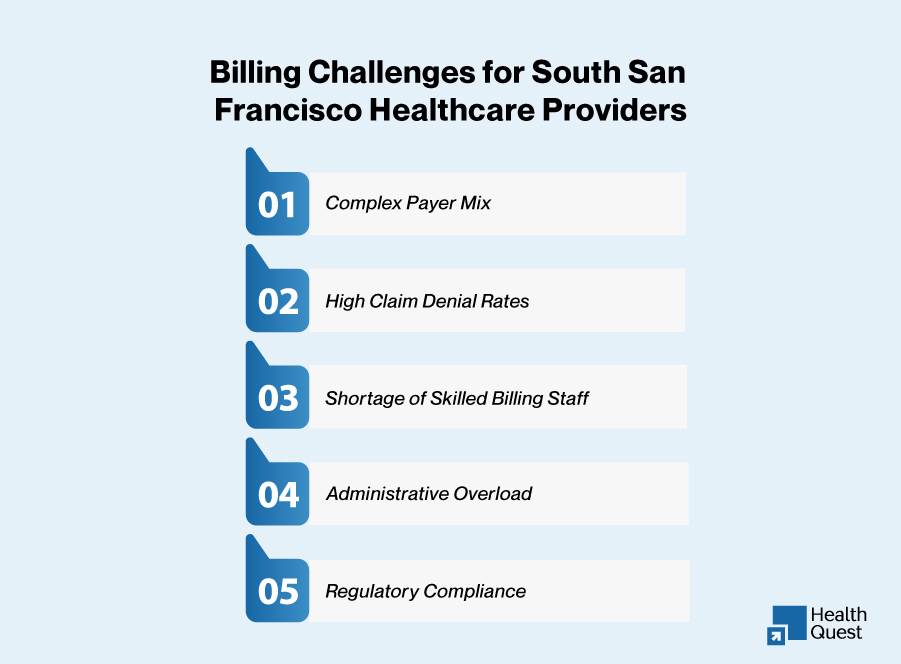
South San Francisco’s healthcare ecosystem is diverse, from primary care clinics to specialty practices. The region’s healthcare providers must navigate a complex payer mix, intricate documentation rules, and the fast-paced changes in insurance regulations. Here are some of the most significant billing challenges:
Complex Payer Mix
With numerous private insurers, Medi-Cal, and commercial payers operating in South San Francisco, each payer has its own set of rules and requirements. Practices must remain updated on these constantly changing guidelines to avoid claim denials.
High Claim Denial Rates
Claim denials can severely impact a practice’s revenue. Incorrect coding, missed modifiers, and eligibility verification errors can lead to delayed reimbursements or even lost revenue.
Shortage of Skilled Billing Staff
The shortage of qualified medical billing professionals is a widespread issue, especially in smaller practices and rural areas. Practices often struggle to find skilled staff to handle complex billing tasks, leading to errors and inefficiencies.
Administrative Overload
Managing prior authorizations, coding updates, and follow-ups with payers can overwhelm office staff, diverting their attention from patient care and increasing the likelihood of errors.
Regulatory Compliance
Practices must comply with both federal regulations and California-specific rules like Medi-Cal and other state insurance programs. This requires ongoing staff training and system updates to avoid penalties.
Navigating the Complex Healthcare Landscape in South San Francisco
The healthcare environment in South San Francisco is characterized by a wide variety of specialties, from urgent care centers to behavioral health providers and complex surgical practices. Understanding the unique billing needs of each specialty is critical to ensuring proper reimbursement.
Specialty-Specific Billing Challenges
From behavioral health’s strict documentation requirements to cardiology’s need for precise modifier usage, each specialty has its own set of billing nuances. Partnering with a billing service experienced in your specialty can improve accuracy, reduce denials, and speed up reimbursement cycles.
Payer Behavior and Bundling
Each payer, whether commercial or public (like Medi-Cal), has its own set of rules, particularly around bundled payments and prior authorizations. Properly navigating these requirements is essential to avoiding revenue losses.
California-Specific Regulations
California’s healthcare landscape comes with its own set of challenges. Practices must adhere to Medi-Cal rules, Medicaid expansion, and other state-specific guidelines. Non-compliance can lead to penalties, denied claims, and delays in payment.
The Real Drivers Behind Revenue Losses in 2025
While declining patient volumes are often cited as a reason for financial strain, inefficiencies in billing are the real culprit for many practices. Some of the most significant drivers of revenue loss in South San Francisco include:
- Payer Policy Changes: Constantly evolving policies can lead to denied or underpaid claims if practices fail to stay updated.
- Rising Documentation Standards: As payers become more stringent, documentation errors are more likely to result in denials.
- Aging Accounts Receivable: Unresolved claims that age past 30 or 60 days become harder to collect and reduce overall cash flow.
- Administrative Burden: In-house billing takes valuable time away from staff, resulting in burnout and increased potential for mistakes.
Read: Best Medical Billing Company in Massachusetts: Streamlining Revenue for Clinics & Hospitals
How Outsourcing Medical Billing Can Help
By outsourcing medical billing to a professional service, practices in South San Francisco can alleviate these challenges and focus on patient care. Here’s how outsourcing benefits practices:
Cost Efficiency and Scalability
Outsourcing eliminates the need for in-house billing staff, training, and software costs. Billing services scale according to your practice’s growth, ensuring that billing tasks are handled efficiently regardless of patient volume or seasonal fluctuations.
Expertise in Navigating Local Payer Rules
Outsourced billing services are well-versed in the specific payer rules for South San Francisco’s healthcare providers. They understand the intricacies of Medi-Cal, commercial payers, and Medicare, ensuring that your claims are submitted correctly and on time.
Proactive Denial Management
Medical billing services handle denial management proactively, tracking claims and resolving issues before they affect cash flow. This reduces administrative stress and ensures that reimbursements are received faster.
Compliance and Risk Management
Outsourcing billing ensures that your practice remains compliant with both federal and state regulations. Billing experts stay updated on regulatory changes, helping your practice avoid penalties and audits.
Nationwide Trends, Local Expertise
While the challenges in South San Francisco may feel unique, they echo nationwide. Medical billing companies with a national presence, yet local expertise, offer the best of both worlds by providing broader payer insights into local practices. For example, billing for cardiology in New York might involve similar coding challenges, but the payer policies differ vastly between states.
Across the country, states like California, New York, Ohio, Florida, and Indiana are witnessing a rise in denials tied to specialty-specific gaps. As the billing landscape becomes more sophisticated, providers are increasingly turning to outsourced medical billing solutions that align with their clinical focus and state regulations.
This shift is not just about convenience, it’s about survival in an environment where payer edits become stricter, documentation reviews increase, and small errors lead to denials. Below is a table summarizing what practices need to be watched:
| Trend | Details | Billing Implications | Best Practices |
| Medicaid Managed Care | Most Medi-Cal patients are enrolled in managed care plans. | Each plan has specific rules for authorizations and documentation. | Keep an updated payer matrix and use automated tools for pre-auth tracking. |
| Commercial Payers | Insurance providers like Anthem and Blue Shield impose strict documentation. | Claims lacking sufficient clinical info are often denied. | Verify benefits and pre-auth requirements before service. |
| Telehealth Coverage Variability | Telehealth services require different coding for video, audio-only, or asynchronous. | Inconsistent coding leads to underpayments or denials. | Maintain a list of payer-specific telehealth coding rules. |
| Audit Pressure from Payers | Increased audits, especially for high-risk services and outliers. | Missing or vague documentation can trigger audits or recoupment. | Conduct internal audits monthly and educate staff on documentation. |
Policy Updates to Watch in 2026
As we approach 2026, several important policy updates are expected to impact medical billing services for healthcare providers in South San Francisco. Keeping up-to-date with these changes is crucial to maintaining compliance and optimizing reimbursement rates. Key updates to watch include:
- California-Specific Changes: Updates in Medi-Cal rules and coverage adjustments.
- Telehealth Reimbursement: Continued expansion or limitation of reimbursement for telehealth services depending on payer policies.
- Medicaid Redetermination: Continued changes in Medicaid eligibility and coverage for state programs.
- Federal Regulations: Changes in the No Surprises Act and other federal compliance issues related to out-of-network billing.
Specialty Billing Isn’t One-Size-Fits-All
In South San Francisco, as across the country, different medical specialties face unique billing challenges. For instance, practices in dermatology, cardiology, behavioral health, and urgent care all encounter distinct payer requirements. Customizing billing services to each specialty’s needs ensures a higher rate of claim approval and more predictable revenue cycles. Without tailored billing, practices may experience underpayments, rejected claims, and unnecessary delays.
Comparing In-House vs. Outsourced Medical Billing
In-House Medical Billing
- Pros: Full control over billing processes and staff.
- Cons: High overhead costs, difficulty staying compliant with payer updates, and potential billing errors due to staffing issues.
Outsourced Medical Billing
- Pros: Lower overhead costs, specialized expertise in managing complex billing and coding, proactive denial management and scalability with practice growth.
- Cons: Less direct control over billing processes but with real-time access to performance reports.
Outsourcing billing services offers practices the ability to focus on patient care while improving billing accuracy, compliance, and cash flow.
How to Choose the Best Medical Billing Partner in South San Francisco
When selecting a billing service, it’s important to choose one that understands both your specialty and the local healthcare market. Here’s what to look for:
Local Expertise
A billing service with experience in the South San Francisco healthcare market is essential. They should understand the payer landscape, including Medi-Cal, commercial insurance, and Medicare.
Specialty-Specific Knowledge
Choose a reliable medical billing service near you, whether it’s urgent care, cardiology, dermatology, or behavioral health. Specialized services ensure that claims are handled correctly, reducing denials and speeding up reimbursements.
Transparent Reporting
Your billing service should provide clear performance metrics, including first-pass claim resolution rates, denial rates, and average days in accounts receivable.
Scalability and Customization
Look for a billing company that can grow with your practice and customize its services to meet your specific needs. This is particularly important if your practice plans to expand or introduce new services.
Top Billing Services Provided by Health Quest Billing for Healthcare Providers in South San Francisco
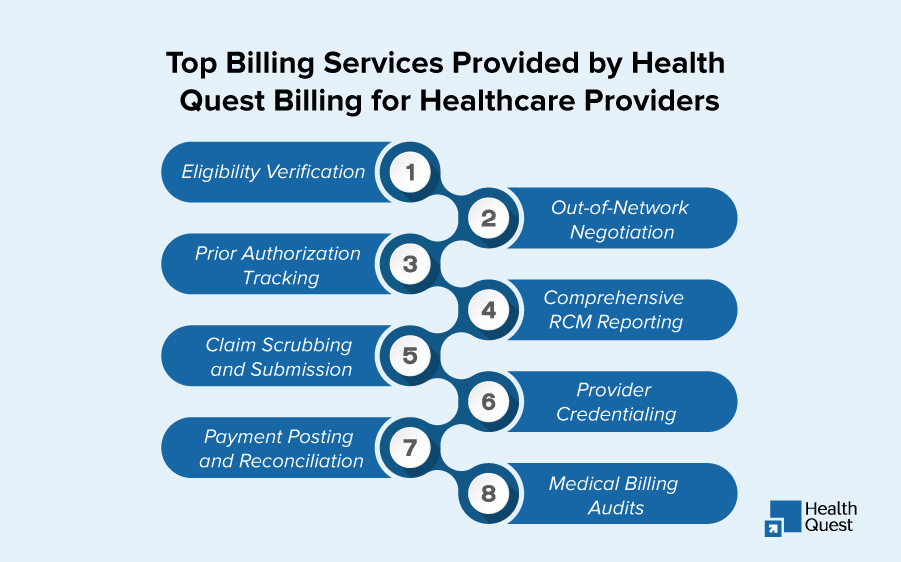
To help healthcare providers in South San Francisco stay competitive and optimize their financial operations, Health Quest Billing offers a comprehensive suite of specialized medical billing services. These services are designed to streamline the revenue cycle, reduce claim denials, ensure compliance with payer policies, and enhance overall cash flow. The following services are essential for maintaining financial health:
- Eligibility Verification
Health Quest Billing ensures that your practice verifies patient insurance coverage in real time, preventing billing issues before they arise. With up-to-date verification, we help ensure that your claims are submitted with accurate payer information, reducing the risk of denials and improving first-pass acceptance rates. - Prior Authorization Tracking
Navigating the complexities of prior authorization requirements can be challenging. At Health Quest Billing, we efficiently track and manage prior authorizations for your practice, ensuring that all necessary approvals are obtained before services are rendered, helping to avoid delays and prevent claim rejections. - Claim Scrubbing and Submission
Health Quest Billing performs thorough claim scrubbing to identify and correct any coding errors, missing information, or formatting issues before submission. This meticulous process reduces the chances of claim denials, accelerates reimbursement cycles, and minimizes rework for your practice. - Payment Posting and Reconciliation
Our team ensures that payments from insurance companies and patients are accurately posted to your practice’s system, and we perform detailed reconciliations to match payments with outstanding balances. This process allows us to quickly identify and address discrepancies, maintaining a healthy cash flow for your practice. - Out-of-Network Negotiation
For providers who work with out-of-network insurance companies, Health Quest Billing offers expert negotiation services to secure fair and adequate reimbursement. We handle the complex task of negotiating reimbursement rates, ensuring that your practice is compensated appropriately for the services you provide. - Comprehensive RCM (Revenue Cycle Management) Reporting
Health Quest Billing provides in-depth financial reporting to give your practice clear insights into the health of your revenue cycle. From denial trends to accounts receivable performance, our reports help identify areas for improvement, optimize billing processes, and support data-driven decision-making. - Provider Credentialing
We streamline the provider credentialing process to ensure that new providers are fully enrolled and eligible to bill insurance companies as quickly as possible. Health Quest Billing helps your practice stay compliant with payer requirements and reduces the risk of denied claims due to credentialing delays or errors. - Medical Billing Audits
Regular audits are essential for maintaining compliance and accuracy in your billing practices. Health Quest Billing offers comprehensive medical billing audits that identify potential errors or risks, ensuring that your practice stays up to date with the latest coding requirements and payer policies, while avoiding costly penalties or audits.
Final Thoughts
Medical billing is a critical aspect of financial health for healthcare providers in South San Francisco. By outsourcing billing to a trusted partner, practices can reduce administrative burdens, improve reimbursement rates, and stay compliant with changing regulations. If your practice is struggling with billing inefficiencies, partnering with a professional billing service can provide the support you need to focus on what matters most delivering excellent patient care.