Otolaryngology (ENT) practices across the United States face one of the most complex billing landscapes in healthcare. With a mix of surgical procedures, in-office treatments, diagnostics, audiology, allergy services, endoscopies, and multi-modality visits, ENT billing requires precision, specialty-specific expertise, and strong payer navigation.
As reimbursement rules tighten, denials increase, and payer audits intensify, ENT clinics can no longer rely on outdated billing workflows. The cost of poor ENT billing is enormous and often invisible until AR days spike or revenue drops unexpectedly.
In 2024, ENT practices reported:
- 18–32% denial rates across major states (TX, FL, CA, NY, OH, GA)
- 25–40% of denied ENT claims linked to coding errors (AAO-HNS 2024
- $78,000–$240,000 annual revenue leakage for small ENT practices due to billing inefficiencies
- Longer payment cycles for endoscopy, allergy immunotherapy & sinus surgeries
This growing complexity makes specialty-focused Otolaryngology Billing and Coding Services essential for stable revenue, predictable cash flow, and long-term practice sustainability.
Why ENT Billing Matters More Than Ever in 2025
Otolaryngology is one of the fastest-evolving specialties in outpatient care. New technologies, image-guided surgeries, allergy treatments, audiology regulations, and sinus procedures have reshaped how clinics bill and how payers respond.
In 2025, ENT practices face:
- Higher denial rates for sinus surgeries, endoscopies, and balloon sinuplasty
- Strict documentation standards for E/M services
- Bundling & unbundling confusion for multi-service visits
- More prior authorizations for sleep apnea testing, allergy services, and advanced imaging
- Increased payer scrutiny for modifier use (especially 25, 59, 52, and XS)
- Rising volume of patient responsibility due to high-deductible plans
States like Texas, Florida, New York, Arizona, and Pennsylvania report the highest ENT claim denial increases in 2024–2025.
Without streamlined ENT billing strategies, practices lose revenue before they even realize what went wrong.
Common ENT Billing Challenges
Otolaryngology billing is uniquely difficult due to the diversity of services. A single patient encounter may include:
- Diagnostic endoscopy
- E/M visit
- Nasal endoscopy with biopsy
- Audiology tests
- Allergy testing
- Sinus irrigation
- Laryngoscopy
Each service has unique CPT/ICD-10 rules, modifier requirements, and payer limitations.
Top ENT Billing Pain Points:
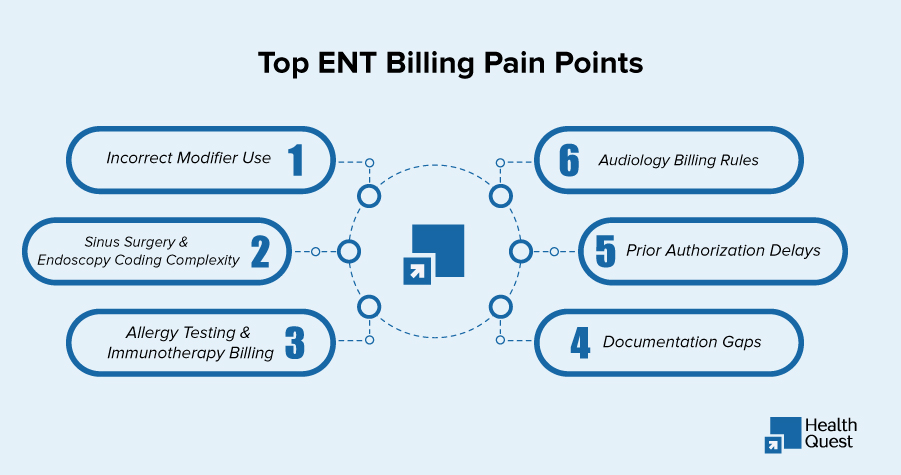
1. Incorrect Modifier Use
Most common ENT modifier issues include:
- Modifier 25 for E/M + procedure
- Modifier 59/XS for separate anatomical sites
- Modifier 52 for reduced services
- Modifier 22 for increased procedural services
Missing or incorrect modifiers lead to 18–24% preventable denials.
2. Sinus Surgery & Endoscopy Coding Complexity
CPT codes for nasal/sinus endoscopy are among the most frequently denied ENT codes nationwide.
3. Allergy Testing & Immunotherapy Billing
Allergy billing rules differ by state and payer, especially regarding:
- Vial preparation
- Injection frequency
- Supervision requirements
- Global periods
4. Audiology Billing Rules
Medicare and Medicaid impose unique coverage restrictions for:
- Hearing aid evaluations
- Audiometry
- Cochlear implant services
5. Prior Authorization Delays
Procedures requiring PA:
- CT scans
- Sleep studies
- Balloon sinuplasty
- Sinus surgeries
- Allergy treatments
- Tympanostomy
6. Documentation Gaps
Most ENT denials stem from incomplete documentation for:
- Medical necessity
- Scope findings
- Biopsy justification
- Anatomical specificity
ENT Billing & Coding Must-Know Trends for 2025
To optimize revenue, ENT practices must understand 2025 shifts:
1. Medicare’s updated E/M guidelines
Improper E/M leveling is a major denial driver.
2. Increase in prepayment audits for ENT procedures
Especially in NY, CA, TX, FL, and NJ.
3. Bundling rules tightening
Sinus surgery + endoscopy unbundling is under heavy review.
4. Higher patient out-of-pocket costs
ENT clinics must enhance patient eligibility and estimates to prevent bad debt.
5. Greater scrutiny of CPT codes:
31231, 31237, 31253–31298, 92557, 95165, 99214–99215.
ENT Coding Breakdown Table
| Category | Examples | Common Coding Issues |
| Endoscopy | 31231, 31233, 31237 | Bundling, missing modifiers |
| Sinus Surgery | 31253–31298 | Medical necessity + PA |
| Audiology | 92557, 92567, 92626 | Medicare restrictions |
| Allergy Services | 95165, 95117, 95180 | Incorrect vial billing |
| Sleep Studies | 95806, 95810 | PA + justification |
| E/M Services | 99213–99215 | Incorrect leveling |
Why ENT Clinics Lose Money?
Most ENT clinics don’t track these hidden revenue leaks:
- Missed charges in endoscopy documentation
- Under-coded E/M visits
- Overlooked audiology tests
- Incorrect allergy vial billing
- Lost surgery revenue due to PA errors
- Failure to appeal ENT-specific denials
- AR days are creeping past 45–60 days
- No tracking of payer underpayments
These issues can quietly drain 10–25% of annual revenue from ENT clinics.
How Health Quest Billing Helps ENT Practices
 Health Quest Billing supports Otolaryngology practices by:
Health Quest Billing supports Otolaryngology practices by:
- Conducting ENT-specific coding audits
- Strengthening modifier accuracy
- Managing prior authorizations for ENT surgeries
- Improving ENT charge capture
- Reducing denials for sinus surgery, endoscopy & allergy services
- Optimizing audiology billing compliance
- Reducing AR days with specialty workflows
- Providing state-level payer guidance
- Offering real-time reporting on ENT KPIs
- Ensuring adherence to CMS & AAO-HNS guidelines
We work with ENT practices across:
Texas, Florida, New York, California, Illinois, Georgia, Pennsylvania, North Carolina, Arizona, and more.
Key Takeaway
Otolaryngology billing is one of the most specialized and revenue-sensitive areas of healthcare billing.
Without a structured, specialty-trained billing partner, ENT practices risk:
- Higher denials
- Lower collections
- Lost surgical revenue
- Compliance risks
- Slower cash flow
- Operational burnout
But with the right support and the right ENT billing strategy, clinics can increase collections, stabilize revenue, and improve patient access to care.
And that’s where Health Quest Billing becomes your competitive advantage.