Plastic surgery remains one of the most financially significant specialties in healthcare, but it also continues to be one of the most challenging from a billing and reimbursement perspective. In 2026, plastic surgery billing services require more than just claim submission; it demands a deep understanding of plastic surgery medical billing, including advanced technology, precise coding, and meticulous documentation. Without specialized expertise in plastic surgery coding, clinics risk compliance issues, delayed payments, and significant revenue loss.
With ongoing payer policy evolution, the expansion of AI-driven claims processing, and changing patient expectations, plastic surgery practices must navigate these complexities to ensure their revenue cycle management for plastic surgeons is efficient and profitable.
What Is Plastic Surgery Billing?
Plastic surgery billing is the process of managing the revenue cycle for cosmetic surgery billing and reconstructive surgery billing. This includes verifying coverage, submitting claims, posting payments, and handling denials. Plastic surgery medical billing is unique in that it involves services that are medically necessary (reconstructive surgeries) as well as elective (cosmetic surgeries), each governed by different billing standards.
Unlike many other medical specialties, plastic surgery billing services must ensure that the distinction between reconstructive surgery (covered by insurance) and cosmetic surgery (typically self-pay) is clear, as these procedures have distinct requirements and pricing structures.
Key Components of Plastic & Reconstructive Surgery Billing in 2026
In 2026, the revenue cycle management for plastic surgeons includes several critical steps. Each phase plays a vital role in maximizing reimbursement and minimizing denials.
1. Insurance Verification and Benefits Investigation
This initial step is crucial in plastic surgery medical billing. Insurance verification ensures coverage for reconstructive surgery billing, such as breast reconstruction after mastectomy or functional rhinoplasty. Verifying eligibility and understanding coverage limitations helps avoid denials related to coverage mismatches or insufficient benefits.
2. Prior Authorization
For reconstructive services, prior authorization is often essential. In 2026, studies show that Medicare Advantage plans denied approximately 7.7% of prior authorization requests in 2024. The increased complexity of prior authorization for plastic surgery emphasizes the need for proactive management and documentation to avoid delays and denials for surgeries like breast reduction or functional nasal reconstruction.
3. CPT and ICD-10 Coding Accuracy
Correct plastic surgery coding is the backbone of effective plastic surgery billing services. Many plastic surgeries involve multiple procedures in one session, requiring proper use of CPT codes and ICD-10 diagnoses. Proper use of modifiers to reflect additional procedures or staged surgeries is essential to prevent bundling issues or underpayment.
5. Claim Submission and Payer Compliance
Each payer has unique requirements, making plastic surgery medical billing a complex process. Claims must meet payer-specific standards, especially with insurers increasingly using AI to flag inconsistencies in documentation or coding. Ensuring compliance with payer guidelines is essential to prevent denials.
6. Payment Posting, Reconciliation, and AR Management
Once processed, payments for plastic surgery procedures must be posted, reconciled against contracted rates, and monitored to ensure that they match what was expected. Aging accounts receivable can result from delays in posting payments or discrepancies, leading to cash flow issues for clinics.
7. Denial and Appeal Management
With growing payer scrutiny, managing denials has become a critical part of plastic surgery revenue cycle management. Denial management in plastic surgery involves identifying trends in denials, addressing root causes, and ensuring the timely submission of appeals with comprehensive documentation to recover lost revenue.
Why Plastic Surgery Billing Is Uniquely Complex
Plastic surgery billing is especially complex because it straddles the line between cosmetic procedures and reconstructive surgeries. The distinctions between these two service types are crucial for correct billing.
- AI and Automation: Insurers increasingly use AI tools to detect errors in claims processing, which could lead to denials or payment reductions. A slight error in plastic surgery coding can trigger denials, affecting reimbursement.
- Global Surgical Periods: Many procedures in plastic surgery involve global periods (post-surgery care included). Billing follow-up procedures or revision surgeries during this period requires careful use of modifiers to avoid confusion with standard post-operative care.
- Cosmetic vs. Reconstructive Services: Incorrectly categorizing a cosmetic procedure as reconstructive surgery can lead to significant financial penalties. Proper documentation for cosmetic surgery billing ensures compliance with payer requirements and financial transparency.
The True Cost of Denials in Plastic Surgery
Denial management in plastic surgery is a critical part of maintaining financial health for your practice. Denied claims don’t just represent a loss of revenue; they result in substantial additional costs for rework, administrative time, and potential audits. For example, a denied reconstructive surgery claim can delay the reimbursement of $8,000 to $15,000 or more.
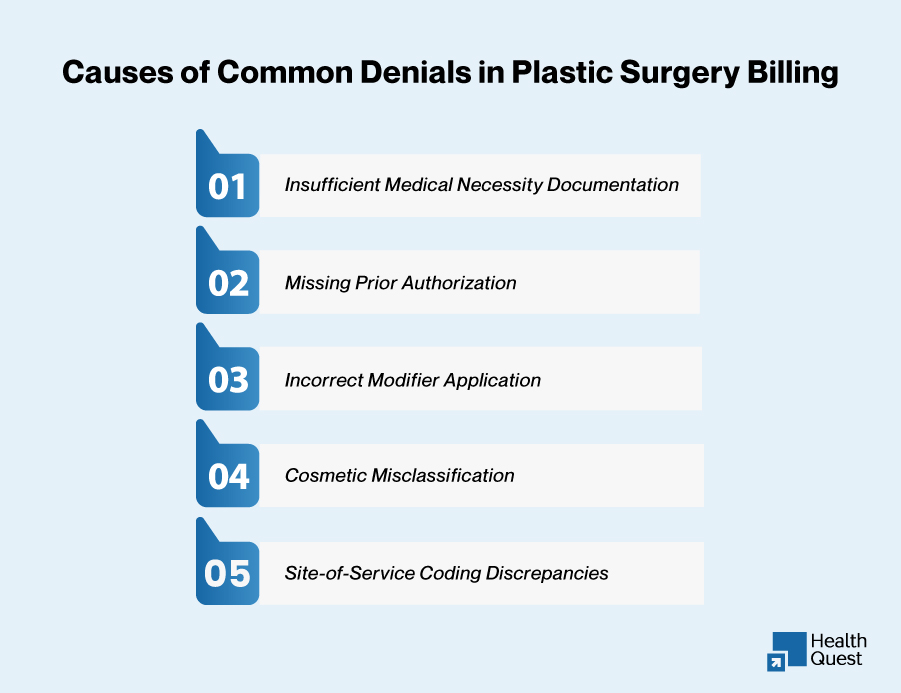
Common Denial Causes Include:
- Insufficient medical necessity documentation: Not providing enough clinical evidence to justify reconstructive surgeries.
- Missing prior authorization: Failure to obtain approval before performing services.
- Incorrect modifier application: Using improper modifiers for complex multi-procedure surgeries.
- Cosmetic misclassification: Mislabeling a reconstructive surgery as cosmetic, leading to self-pay billing and potential audits.
- Site-of-service coding discrepancies: Incorrect assignment of procedures to outpatient settings when they should be inpatient.
Beyond delayed revenue, repeated denials increase administrative workload and raise audit risk. The true cost of denials isn’t only the lost revenue but also the potential for future payer scrutiny, leading to even more challenges. This is why proactive denial management in plastic surgery is essential, focusing on root cause analysis and prevention rather than just appeal submission.
2026 CMS Updates and Their Impact on Plastic Surgery Billing
Several CMS updates introduced in 2026 have significant implications for plastic surgery billing services. The Centers for Medicare & Medicaid Services (CMS) finalized several critical changes that plastic surgery practices need to be aware of:
-
Medicare Physician Fee Schedule (PFS) Changes
CMS introduced a 3.26% increase in the base conversion factor, which is beneficial for many procedures. However, there was also a –2.5% efficiency adjustment for non-time-based services, impacting some plastic surgery codes. These changes highlight the need for precise plastic surgery coding and medical billing services to avoid underpayment.
-
Prior Authorization Expansion
CMS has expanded prior authorization requirements for reconstructive surgeries like breast reconstruction, functional rhinoplasty, and skin excision after weight loss. Prior authorization is more strictly enforced, particularly for these high-value procedures.
-
Increased Scrutiny of Site-of-Service Codes
CMS has introduced stricter guidelines on site-of-service codes, reviewing ASC vs. inpatient settings for certain plastic surgeries. This change emphasizes the need for careful site-of-service documentation in plastic surgery medical billing.
State-Specific Plastic Surgery Billing Considerations: Revenue Risk and Financial Impact
In 2026, state-specific regulations are increasingly important for plastic surgery practices. States with high volumes of procedures, such as California, Texas, and Florida, have introduced stricter prior authorization requirements and payer scrutiny. Failure to comply with these state regulations can lead to significant revenue loss and delayed reimbursements.
Here’s how state-level changes pose revenue risks and the financial consequences of non-compliance:
| State | Impact of Changes | Revenue Risk & Financial Consequences |
| California | Prior authorization for more reconstructive procedures. | $8,000 – $12,000 lost per claim due to delayed prior authorization. |
| Texas | Expanded prior authorization for breast reductions. | $10,000 in lost revenue per procedure if prior authorization is denied. |
| Florida | Scrutiny on cosmetic procedures during global periods. | 15-20% revenue loss per claim for facelifts and body contouring. |
| Pennsylvania | CMS review for elective procedures. | $10,000+ in fines and denial penalties for misclassified services. |
| New York | New prior authorization for skin excisions post-weight loss. | $7,000 – $12,000 delayed for panniculectomy claims. |
| Ohio | Prior authorization for both cosmetic and reconstructive surgeries. | $10,000 per claim lost due to incomplete authorizations. |
| Georgia | Tighter documentation for hybrid surgeries. | 10-15% revenue leakage for improperly categorized hybrid surgeries. |
These changes directly impact revenue cycle management. Practices must automate prior authorization tracking, ensure accurate documentation, and stay updated on payer policy changes to mitigate financial risks. Non-compliance can lead to substantial revenue loss, with some practices losing up to 20% of their annual revenue.
The Biggest Revenue Threats Plastic Surgery Practices Face in 2026
As payer expectations shift, plastic surgery practices face several key revenue cycle risks:
- Medical Necessity Denials: Insufficient documentation for reconstructive procedures can lead to denials.
- Prior Authorization Failures: The increasing complexity of prior authorization for plastic surgery demands timely submission and precise documentation.
- Efficiency Adjustments by CMS: Reimbursement reductions due to CMS efficiency adjustments may impact certain plastic surgery procedures.
- Underpayments: Payer discrepancies can affect practice profitability, requiring careful payer contract management.
Best Practices to Ensure Revenue Protection in Plastic Surgery Billing (2026)
To protect revenue cycle integrity, plastic surgery billing services should follow best practices like:
- Quarterly Documentation Audits to ensure compliance.
- Automated Prior Authorization Systems to track approvals efficiently.
- AI-Assisted Claim Scrubbing to reduce coding errors before submission.
- Payer Monitoring to adapt quickly to changing payer rules.
Why Outsource Plastic Surgery Billing Services?
Outsourcing your plastic surgery billing services to a specialized provider can deliver numerous advantages, allowing your practice to focus on what matters most: patient care and growing your practice. Here’s why you should consider outsourcing:
- Specialized Expertise: An experienced medical billing company for plastic surgeons understands the nuances of both cosmetic surgery billing and reconstructive surgery billing. Outsourcing ensures accurate and compliant coding, reducing the risk of denials.
- Cost-Effective: Outsourcing plastic surgery billing services can lower overhead costs by eliminating the need for in-house billing staff, training, and technology investments.
- Faster Reimbursements: By working with professionals who specialize in denial management in plastic surgery, outsourced billing partners can identify and resolve issues faster, ensuring quicker reimbursements and less disruption to cash flow.
- Focus on Patient Care: With an expert billing team managing your claims, you can dedicate more time to delivering high-quality care and growing your patient base.
By outsourcing your plastic surgery medical billing, you free up time to focus on improving your patient outcomes and growing your practice, while a trusted partner takes care of the revenue cycle complexities.
How Health Quest Billing Supports Plastic Surgery Practices in 2026

At Health Quest Billing, we offer customized plastic surgery billing solutions tailored to meet the unique needs of your practice. Our services are designed to streamline your revenue cycle, reduce inefficiencies, and enhance profitability. We specialize in:
- Real-time Eligibility Verification & Prior Authorization Management:
Ensuring timely approvals and minimizing delays by verifying coverage and managing pre-surgical authorizations.
- Expert CPT & ICD-10 Coding:
Providing precise coding for both cosmetic and reconstructive procedures to ensure accurate reimbursements and avoid claim rejections.
- Proactive Denial Management & Payer Communication:
Quickly identifying and addressing denials with comprehensive appeal strategies, ensuring your practice recovers lost revenue.
- Comprehensive Financial Reporting & KPI Monitoring:
Offering real-time insights into your practice’s financial performance, allowing you to make informed decisions and optimize cash flow.
- Full Compliance with CMS & State Regulations:
Keeping your practice up-to-date with the latest regulatory changes to maintain compliance and avoid costly penalties.
Our plastic surgery billing services are crafted to minimize denial rates, accelerate reimbursements, and ensure your practice remains compliant with evolving coding standards. Trust us to manage your billing, so you can focus on delivering exceptional patient care.
Conclusion
In 2026, plastic surgery billing is more complex than ever before. Practices must stay ahead of changes in CMS policies, prior authorization regulations, and evolving payer requirements. Partnering with a trusted medical billing company for plastic surgeons, like Health Quest Billing allows you to optimize your revenue cycle management, reduce denials, and maximize financial growth while staying compliant.
Contact Health Quest Billing today to streamline your plastic surgery medical billing process and secure long-term financial stability in 2026.