Credentialing healthcare providers is essential for ensuring they are qualified to deliver safe and effective care. This process verifies key qualifications, including education, licensure, board certifications, and malpractice insurance. A study in the Journal of the American Medical Association (JAMA) found that strong credentialing practices reduced adverse events by 20% and preventable medical errors by 15%, underscoring its importance in patient safety.
However, credentialing is an ongoing process that requires regular updates and monitoring. Providers must maintain their qualifications to ensure continued compliance. Hospitals with comprehensive credentialing programs report up to 30% fewer malpractice claims. In this guide, we’ll explore the credentialing process, common challenges, and best practices to help you maintain a qualified healthcare workforce.
What is credentialing for Primary care and specialty care?
Credentialing ensures that primary and specialty care providers are qualified to deliver safe care. For primary care providers, this means verifying their education, licensure, and residency training. For specialists, it includes additional checks like board certifications and specific experience in their field. The process also involves peer reviews and regular re-credentialing to keep credentials up to date. Ultimately, credentialing helps maintain high standards and ensures patient safety.
There are several steps in the credentialing process for primary and specialty care services.
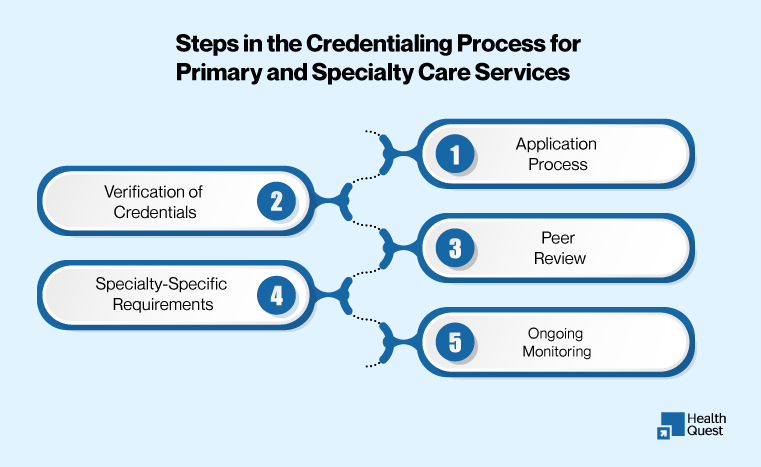
Verification of Credentials:
The first step is to verify the provider’s qualifications by contacting primary sources, such as medical schools, residency programs, licensing boards, and previous employers. This ensures the accuracy of the provider’s educational background, medical licenses, and certifications.
Application Process:
Providers typically submit a detailed application, which includes information on their education, training, work history, professional affiliations, and malpractice insurance coverage.
Specialty-Specific Requirements:
Depending on the provider’s specialty, additional certifications or specific clinical experience may be required. For example, a cardiologist might need to provide proof of specialized training beyond general medical education.
Peer Review:
Some practices involve a peer review process, in which other healthcare professionals assess the provider’s clinical competence and skills.
Ongoing Monitoring:
Credentialing is not a one-time task. Providers must regularly update their credentials and comply with any changes in licensing, certification, or insurance requirements to maintain their eligibility to practice.
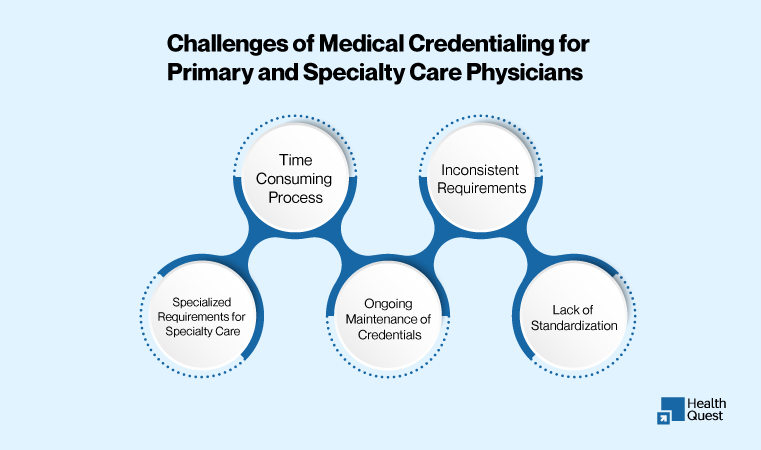
Challenges of Medical Credentialing for Primary and Specialty Care Physicians
-
Time-Consuming Process:
Credentialing requires extensive documentation and verification, often involving multiple sources such as medical schools, residency programs, and licensing boards. This process is lengthy and can delay the onboarding of new physicians.
-
Inconsistent Requirements
Different insurance companies and healthcare organizations may have varying credentialing requirements. This inconsistency creates confusion and adds complexity for physicians who need to meet different standards for each network or practice.
-
Specialized Requirements for Specialty Care
Additional qualifications and certifications are necessary for specialty care physicians. Verifying specialized training, board certifications, and specific clinical experience takes more time and resources than credentialing primary care providers.
-
Ongoing Maintenance of Credentials
Credentialing is not a one-time process; providers should regularly update their credentials, including staff licensure, board certifications, and malpractice insurance. Failing to keep the credentials updated can lead to compliance issues.
-
Lack of Standardization
The absence of efficient and standardized credentialing across the healthcare system might lead to inefficiencies. Each institution or payer may have their own set of rules and criteria; therefore, providers need to stick to them to prevent denials.
How Credentialing Services Address These Challenges:
1. Simplifying the Credentialing Process
Credentialing can be a complicated and time-consuming task, but it doesn’t have to be. By handling all the necessary paperwork and verification, from education to malpractice history, the process becomes much smoother. This means less waiting and a faster turnaround for getting providers on-board.
2. Ensuring Consistency Across Healthcare Networks
It can be frustrating to deal with different requirements from various insurance companies and healthcare systems. Credentialing services help by making sure everything meets the specific needs of each payer, while still keeping things streamlined and consistent.
3. Addressing the Unique Needs of Specialty Care
Specialty care providers often have additional qualifications and certifications. It’s not just about medical school anymore, it’s about making sure all the right training, experience, and certifications are in place. With specialized credentialing services like Health Quest, these details are carefully managed so that specialists stay compliant with all their requirements.
4. Keeping Everything Up to Date
Credentialing isn’t just a one-and-done task; it’s an ongoing process. Keeping track of renewals for licenses, board certifications, and malpractice insurance is key to staying compliant. Having someone take care of these updates and send reminders when things need renewing can save a lot of stress and hassle.
5. Offering Clear Communication and Support
Credentialing can be confusing, but it doesn’t have to be. With a dedicated point of contact, providers and practices can easily get answers and solutions to any issues that pop up. This clear communication helps keep everything on track and makes the entire process much more manageable.
Benefits of Medical Credentialing Services for Primary and Specialty Care Practices
Credentialing is a crucial aspect of running a smooth and compliant healthcare practice. Here are the key benefits of using medical credentialing services:
1. Ensures Provider Qualifications and Compliance
Credentialing services verify that every provider is properly licensed, board-certified, and compliant with regulatory requirements. This helps ensure that your team is always qualified and up to date, minimizes the risk of non-compliance, and guarantees that your team meets industry standards.
2. Speeds Up Provider Onboarding
Credentialing can be time-consuming. Outsourcing it can streamline the onboarding process and get new providers working more quickly. Faster onboarding means more efficient operations and reduced staffing delays.
3. Reduces Risk of Claim Denials
Proper credentialing ensures that your practice meets all insurance and payer requirements, reducing the likelihood of claim denials and delays. It improves the cash flow and fewer re-submissions due to denied claims.
4. Improves Regulatory Compliance
Staying on top of changing regulations can be a challenge. Credentialing services keep your practice up-to-date with the latest legal and insurance requirements. Helps avoid penalties, fines, and compliance issues, keeping your practice in good standing.
5. Ongoing Monitoring and Updates
Credentialing isn’t a one-time process. Services ensure that licenses, certifications, and insurance are always current, with regular reminders and updates. Keeps your practice compliant with minimal administrative effort.
6. Saves Time and Reduces Administrative Burden
Credentialing can be a drain on your practice’s administrative resources. Outsourcing frees up your team to focus on patient care and other critical tasks. It reduces administrative workload and improves overall efficiency.
7. Scalable for Practice Growth
As your practice grows, credentialing services can easily scale with you. Whether you’re adding new providers or expanding to new locations, credentialing remains improved. Supports growth and ensures that all new providers are credentialed quickly and efficiently.
Final Thoughts:
Credentialing is an essential aspect of maintaining a qualified healthcare workforce. By partnering with a credentialing service like Health Quest, healthcare organizations can streamline the process, ensure compliance, and reduce administrative burdens. Whether you’re onboarding new providers or keeping existing ones compliant, Health Quest’s expert services provide peace of mind and improved patient safety. Ready to make credentialing easier?
Contact us today at (415) 508-6537 to learn how we can help!