As we enter 2026, healthcare providers ranging from small private practices to large hospitals are continuing to face an increasingly complex landscape. The challenges that emerged in 2025 are not only persistent but also evolving as new regulations, payer requirements, and shifting patient responsibilities continue to impact the revenue cycle. Navigating these changes while ensuring that billing and reimbursement processes remain efficient is no small feat. Whether it’s the impact of rising healthcare costs, the strain of staffing shortages, or the complexities of new coding systems, providers must adapt quickly to stay financially viable.
In this blog, we will explore the challenges driving revenue loss for healthcare providers and discuss how modern billing fixes can help practices recover their revenue and improve financial health in 2026.
Navigating the Financial Squeeze: Key Billing and Coding Challenges in 2026
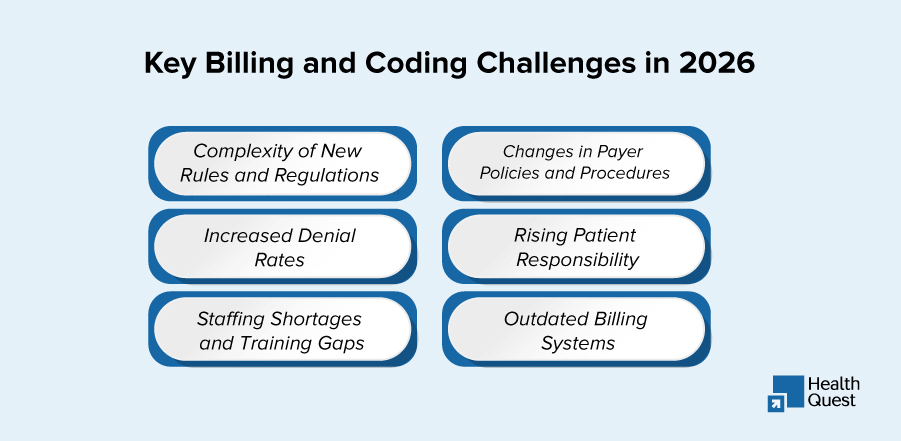
1. Complexity of New Rules and Regulations
The introduction of new rules for coding and billing in 2025 has left many providers scrambling to ensure compliance. With continuous regulatory changes, practices often find themselves out of sync with the latest requirements for reimbursement and coding accuracy. This leads to delayed payments, denials, and missed opportunities for revenue collection.
2. Increased Denial Rates
Claim denials are more prevalent than ever. Insurance companies have become stricter with their claims review processes, making it harder for providers to get reimbursed for the services they deliver. The result is a mountain of denied claims that require extensive time and resources to resolve, ultimately impacting cash flow.
3. Staffing Shortages and Training Gaps
The ongoing staffing shortages within healthcare facilities continue to be a significant issue, leaving billing teams overburdened. As new coding systems and payer guidelines evolve, the burden of ensuring correct billing falls on staff who may not be adequately trained or supported. This leads to revenue leakage as claims are either delayed or underpaid.
4. Changes in Payer Policies and Procedures
Another challenge in 2026 is the continual evolution of payer policies. Insurers often introduce new requirements, such as stricter documentation standards or changes to pre-authorization processes. Without a solid tracking system in place, practices can miss key changes, leading to underpayment or delayed claims, which ultimately harm their revenue stream.
5. Rising Patient Responsibility
As high-deductible health plans (HDHPs) become more common, patients are shouldering a greater portion of their healthcare costs. This shift in financial responsibility means that practices must explore new ways to manage and collect patient payments, placing an additional administrative burden on staff and often leading to delayed or unpaid bills.
6. Outdated Billing Systems
Many practices still rely on outdated billing systems that fail to integrate with modern payer systems. These legacy systems often require manual input and are prone to errors, leading to inefficiencies, delayed claims, and, ultimately, lost revenue.
How Modern Billing Solutions Can Boost Your Practice’s Revenue in 2026
While these challenges are significant, there is hope for healthcare providers. Modern billing solutions offer a comprehensive approach to streamlining the revenue cycle and recovering lost revenue. Let’s explore the tools and strategies that can help practices overcome the hurdles of 2026.
1. The Impact of Data Security and HIPAA Compliance on Revenue Loss
Data breaches and violations of c regulations can result in significant financial penalties, halting revenue flow as practices address security issues. Protecting sensitive patient information is not only a matter of compliance, but it’s also vital for maintaining the financial health of a practice.
To safeguard against revenue loss, practices should:
- Stay updated on security protocols and regularly audit systems for vulnerabilities.
- Invest in cybersecurity tools and staff training to ensure HIPAA compliance.
- Develop a clear breach response plan to minimize disruptions to the billing process.
By ensuring robust data security, practices can avoid penalties that could impede their revenue cycle.
2. The Role of AI and Machine Learning in Optimizing Revenue Cycle Management
AI and machine learning are transforming the way billing processes are handled. These technologies automate administrative tasks such as coding and claims submission, detecting patterns and flagging errors before they affect revenue.
How to Address:
- Integrate AI-powered billing systems that identify claim inaccuracies in real time.
- Use machine learning tools to predict denials and resolve issues proactively.
- Automate coding processes to reduce errors and speed up claims submission.
AI-driven systems can improve billing accuracy, reduce human error, and streamline the reimbursement process.
3. Rising Healthcare Costs: How It Affects Practices’ Bottom Line
The rising costs of healthcare, ranging from staffing to equipment, place a significant financial strain on providers. When reimbursement rates from insurers don’t reflect these increased costs, practices are left with a widening financial gap.
Proven Methods to Address it:
- Negotiate better payer contracts to ensure reimbursement rates align with healthcare costs.
- Implement cost-cutting measures in non-essential areas without affecting patient care.
- Explore value-based care models to improve reimbursement based on patient outcomes.
By optimizing contracts and exploring innovative care models, practices can manage costs without compromising care.
4. The Importance of Accurate Eligibility and Benefits Verification
Incorrect eligibility verification remains a primary cause of claim denials. Practices need to confirm patient eligibility and benefits before rendering services to avoid unnecessary delays in payments.
How to Address:
- Use real-time eligibility verification tools to confirm insurance coverage before services are rendered.
- Implement automated checks to regularly update patient insurance information.
- Educate staff on thoroughly verifying benefits to ensure accurate claim submission.
Accurate eligibility checks help prevent costly errors that lead to denied claims and delayed payments.
5. The Shift Toward Bundled Payments: What Providers Need to Know
Bundled payment models are becoming increasingly common, where providers receive a single payment for a set of services rather than individual reimbursements. Navigating these payment structures requires precision and careful coordination to ensure that all services are adequately covered.
How to Address:
- Understand bundled payment structures and how they impact coding and billing.
- Track and allocate costs effectively within the bundle to ensure proper reimbursement.
- Adapt to performance-based metrics that align with bundled payment goals.
With the right approach, practices can maximize reimbursement from bundled payment models.
6. Patient Communication and Financial Transparency: How It Affects Revenue Collection
Clear communication with patients about their financial responsibilities is key to improving collection rates. Transparent pricing and upfront billing expectations reduce confusion and delays in payments.
How to Address:
- Provide clear and understandable billing statements that outline patient responsibilities.
- Educate patients on financial assistance programs and payment options.
- Use patient-friendly payment portals for easier transactions.
When patients are well-informed about their financial obligations, practices see faster payment collections and fewer disputes.
7. Payer Contract Negotiation: How to Secure Better Rates
Negotiating payer contracts is a powerful tool for improving revenue. Secure contracts with fair reimbursement terms ensure practices are compensated appropriately for the services they provide.
How to Address:
- Regularly review payer contracts and identify areas for improvement.
- Use data analytics to support contract renegotiations and secure higher reimbursement rates.
- Consider seeking expert help for payer negotiations if needed.
By negotiating favorable contracts, practices can secure better reimbursement rates and improve their financial standing.
8. The Role of Financial Analytics in Improving Billing Accuracy
Financial analytics can provide valuable insights into a practice’s revenue cycle performance, helping to identify inefficiencies, track claim trends, and spot revenue leakage.
How to Address:
- Use financial analytics tools to monitor key performance indicators (KPIs).
- Regularly analyze claim denial trends to identify root causes and address them.
- Implement real-time monitoring to spot and resolve issues as they arise.
Using data-driven insights, practices can improve billing accuracy and recover lost revenue.
9. The Growing Importance of Telemedicine and Remote Services Billing
Telehealth services are expanding, but billing for remote care can be tricky. Differences in reimbursement rates, payer policies, and coding for virtual visits make telemedicine billing more complex.
How to Address:
- Stay updated on payer policies for telehealth services.
- Use telemedicine-specific codes for remote visits to ensure proper reimbursement.
- Utilize secure platforms compatible with billing systems for telehealth services.
By mastering telemedicine billing, practices can tap into the growing market for remote care and maximize revenue from these services.
10. Improving Cash Flow Through Strategic Payment Solutions
Strategic payment solutions help streamline collections, improving cash flow. Offering flexible payment options for patients ensures timely payments and reduces outstanding balances.
How to Address:
- Offer flexible payment plans for patients with high out-of-pocket costs.
- Use automated reminders and online payment portals for easier patient payments.
- Provide multiple payment options, including credit card processing and financing options.
By implementing modern payment solutions, practices can reduce patient debt and improve cash flow.
11. The Cost of Inaccurate Coding: How It Can Lead to Revenue Loss
Inaccurate coding is one of the leading causes of claim denials and underpayments. Proper coding is essential to ensure accurate reimbursement for services rendered.
How to Address:
- Conduct regular coding audits to ensure accuracy.
- Provide ongoing training for billing staff to stay current on coding practices.
- Use automated coding systems to reduce human error and improve accuracy.
Accurate coding ensures proper payment and minimizes the risk of costly denials and audits.
How Health Quest Billing Can Help Practices Overcome Revenue Cycle Challenges
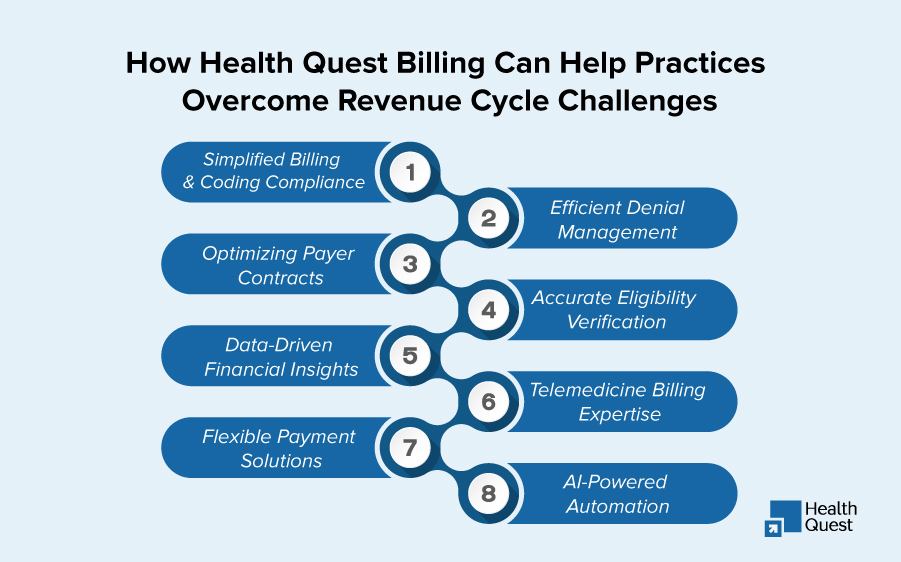
In 2026, healthcare practices face numerous billing challenges, but Health Quest Billing offers expert RCM services to address them directly. Here’s how we can help:
1. Simplified Billing & Coding Compliance
We stay current with the latest regulations and coding changes, ensuring accurate and compliant claims, reducing denials and payment delays.
2. Efficient Denial Management
Our team swiftly resolves denied claims, recovering lost revenue and reducing administrative burdens.
3. Optimizing Payer Contracts
We help negotiate better payer contracts to ensure fair reimbursement rates, maximizing your revenue.
4. Accurate Eligibility Verification
We use real-time eligibility verification tools and automated checks to ensure correct insurance information, minimizing delays and denials.
5. Data-Driven Financial Insights
Our analytics tools track key performance indicators (KPIs), identify revenue leakage, and optimize billing processes for better cash flow.
6. Telemedicine Billing Expertise
We ensure proper reimbursement for telehealth services by using telemedicine-specific codes and staying up-to-date on payer policies.
7. Flexible Payment Solutions
We provide automated payment reminders, online portals, and flexible plans to improve cash flow and reduce patient debt.
8. AI-Powered Automation
We leverage AI tools to automate billing processes, reduce errors, and expedite claims, improving overall efficiency.
Conclusion:
The healthcare industry is constantly evolving, and billing challenges are becoming more complex. But with the right partner, practices can overcome these hurdles and thrive financially. Health Quest Billing offers a tailored approach to revenue cycle management, utilizing the latest technology and expert insights to optimize your billing processes.
If your practice is struggling with rising denial rates, outdated systems, or complex payer requirements, we are here to help. Let us handle your RCM needs so you can focus on what you do best: providing excellent care to your patients.
Take the first step toward financial recovery today. Contact us to learn how our comprehensive RCM services can help your practice streamline billing, reduce errors, and maximize revenue in 2026 and beyond.