Telehealth isn’t just a new trend; it’s a strategic opportunity. For healthcare practices serving Medicaid populations, expanding telehealth offerings translates into increased access for patients and new revenue channels. By billing for live video, audio-only visits, remote patient monitoring (RPM), and asynchronous consultations, providers can boost service volume, reduce no-shows, and reach underserved populations who might otherwise face transportation or mobility barriers. When Medicaid reimbursement policies support these modalities, practices benefit financially while improving care access.
Understanding Medicaid Telehealth Coverage
Medicaid reimbursement varies significantly by state, but most now cover a wide array of telehealth services:
- Live video is reimbursed by all 50 states, plus DC and Puerto Rico, via Medicaid fee-for-service programs.
- Approximately 37 state Medicaid programs reimburse store-and-forward (asynchronous) services, though often with limitations on provider type or service type.
- Remote Patient Monitoring (RPM) is reimbursed by around 42 state programs, with several states having expanded coverage since Fall 2023.
- Audio-only (telephone) visits are reimbursed in about 45 states and DC, though many impose restrictions, such as only for certain services or provider types.
Medicaid treats telehealth as a delivery method, not a separate service. This means Medicaid may reimburse:
- Practitioner fees (CPT/HCPCS codes)
- Distant site fees
- Originating site fees
- Even infrastructure or transmission costs were permitted by state SPAs or waivers
Types of Telehealth Services Covered by Medicaid
Medicaid programs across the U.S. are expanding their telehealth policies to meet rising demand, improve care access, and address provider shortages. Understanding which telehealth modalities are reimbursable in your state can help your practice optimize billing strategies and broaden patient reach, especially in underserved or rural communities.
Live Video
This modality is the most widely reimbursed across Medicaid, permitted in every state program (50 states, DC, PR). However, rules differ around eligible originating sites, provider types, and place-of-service codes.
Store‑and‑Forward (Asynchronous)
Reimbursed in roughly 37 states, this modality supports services that can be delivered without a live encounter, but states like Colorado, Delaware, New Hampshire, and Pennsylvania added limited reimbursement only recently
Remote Patient Monitoring (RPM)
About 42 states reimburse RPM, with expansions underway in several jurisdictions (Delaware, New Hampshire, New Jersey, Pennsylvania, and South Dakota added coverage recently). Provider types and eligible patient conditions vary by state.
Audio‑Only
Telephonic visits are covered in 45 states + DC, often for behavioral health or follow-up care, but the specifics of allowable codes and provider eligibility differ by state
How Medicaid Telehealth Reimbursement Works
Medicaid considers telehealth a delivery method, not a distinct service, meaning states have the power to define how and what they reimburse via State Plan Amendments (SPAs).
Payment Parity & SPAs
States do not need federal approval to reimburse telehealth at the same rate as in-person care. Through SPAs, they decide:
- Covered telehealth services
- Eligible providers
- Reimbursement structures (parity, bundled payments, modality-based rates)
Most states follow flexible models using existing CPT codes, with variations by service type and provider specialty.
What Medicaid Telehealth Fees Are Covered?
States may reimburse one or more of the following under their Medicaid telehealth policies:
- Distant Site Provider Fees: Payment for the provider delivering care via telehealth.
- Originating Site Facility Fees: For the facility or location where the patient is physically located.
- Technology Costs: Some states reimburse for equipment, transmission fees, or technical support either separately or bundled into global payments, depending on SPA language.
Equity & Sustainability Challenges:
While policy flexibility is improving, equity gaps remain in how Medicaid telehealth reimbursement is applied: A study of FQHCs (Federally Qualified Health Centers) in New York revealed that low Medicaid telehealth reimbursement rates were linked to workforce shortages, especially in mental and behavioral health services.
Nationwide, Medicaid beneficiaries remain underrepresented in telehealth utilization despite a 400% increase in total telehealth usage post-pandemic. Barriers include:
- Poor broadband access
- Limited provider participation in Medicaid telehealth
- Digital literacy and technology availability for patients
Medicaid Telehealth Coverage Varies by State
While all state Medicaid programs reimburse for some form of telehealth, coverage details such as which services are eligible and what billing rules apply differ significantly. Some states support full coverage across all modalities (live video, RPM, store-and-forward, and audio-only), while others offer only partial reimbursement or impose strict limitations.
Here’s a brief snapshot of Medicaid telehealth policies in select states:
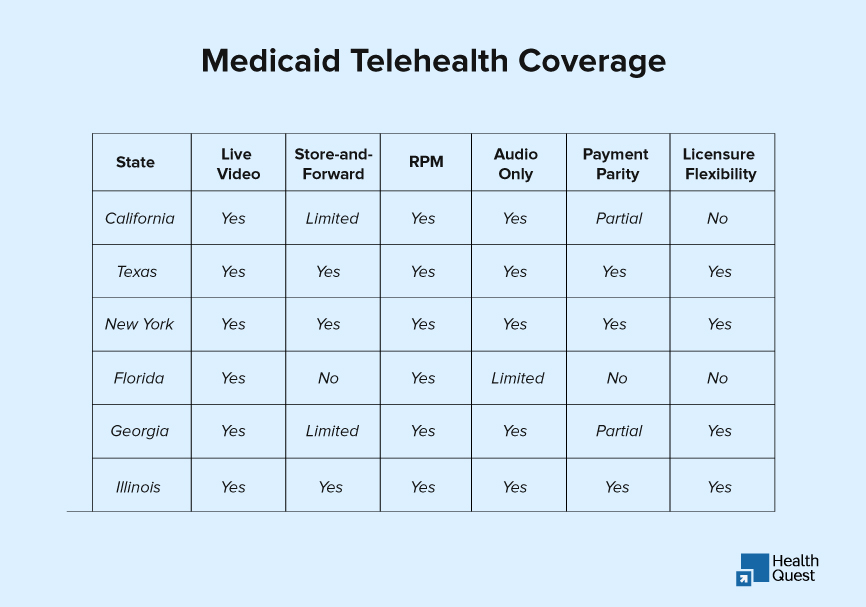
Source: Center for Connected Health Policy – Fall 2024 Medicaid Telehealth Summary Chart (PDF)
How to Bill Medicaid for Telehealth (2025 Edition)
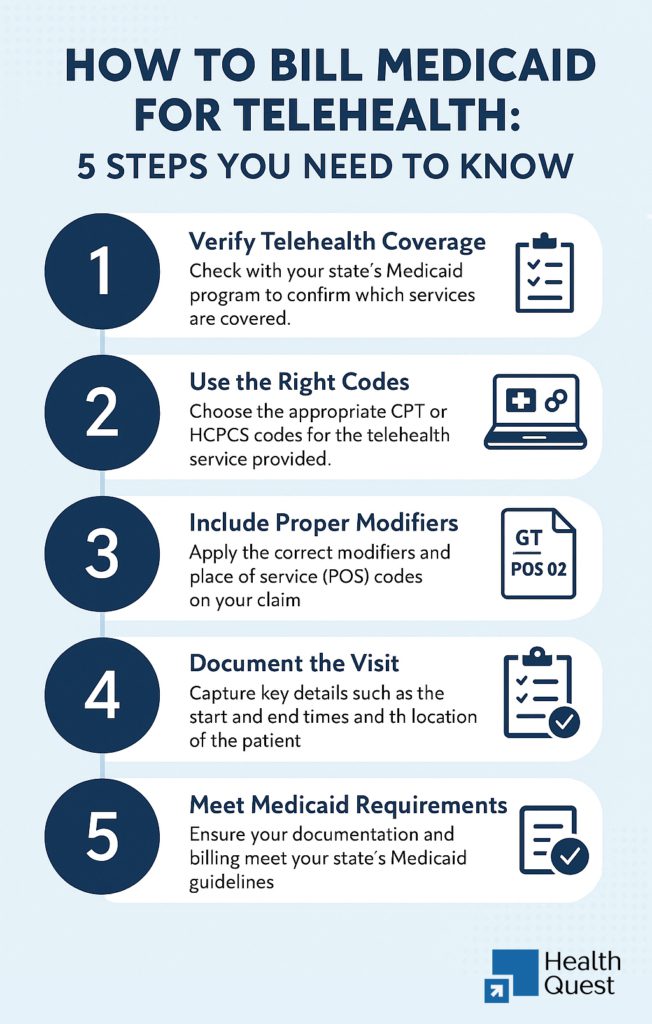
Billing Medicaid for telehealth isn’t just about checking boxes; it’s about getting paid accurately, staying compliant with changing state rules, and making sure your patients get uninterrupted care.
Verify What Your State Medicaid Program Covers
Before you deliver any telehealth service, check your state’s rules. Medicaid telehealth coverage isn’t uniform nationwide.
Here’s what you should look for:
- Which telehealth types are covered: video, audio-only, remote patient monitoring (RPM), or asynchronous (store-and-forward)?
- Who is eligible to bill? Are you a covered provider type?
- Where can the patient be located: Home, school, FQHC, or elsewhere?
- Does your state offer payment parity? Will you be reimbursed the same as an in-person visit?
Use the Correct CPT/HCPCS Codes
Use the same E/M and procedure codes you’d typically use for in-person services unless your state says otherwise.
Common codes:
| 99201–99215: | Office or outpatient visits |
| 99453, 99454, 99457 | Remote patient monitoring |
| H0038, H0046 | Behavioral telehealth in some Medicaid plans |
Apply the Right Modifiers
Modifiers are essential for signaling that a service was delivered via telehealth. They impact how your claim is processed and whether it’s denied.
Frequently used telehealth modifiers:
- 95: Real-time audio and video
- GT: Real-time telehealth via interactive tech (used in legacy systems)
- GQ: Store-and-forward (asynchronous)
- FQ and FY: Audio-only telehealth (used in several states in 2024–2025)
Choose the Correct Place of Service (POS) Code
POS codes help Medicaid identify where the service was provided, and this affects how you’re paid.
Most common POS codes for telehealth:
- POS 02: Telehealth from anywhere other than the patient’s home
- POS 10: Telehealth provided in the patient’s home
Document Everything (Yes, Everything)
Even with the correct codes and modifiers, you can still be denied if your documentation isn’t complete. Make sure to note where the provider and patient were during the visit, and what was the mode of communication?. Patient consent for telehealth and the time of visit are very important to note, along with the details of medical necessity.
Compliance and Audit Considerations: Stay Protected When Billing Telehealth
When billing Medicaid for telehealth, compliance matters just as much as clinical care. Here’s what your practice should keep in mind:
HIPAA-Compliant Tech Is a Must
Use telehealth platforms that meet HIPAA standards, including end-to-end encryption, secure data storage, and Business Associate Agreements (BAAs), which are non-negotiable. Most states no longer allow non-secure tools post-COVID waivers.
Medicaid Documentation Requirements
To stay audit-ready, make sure each telehealth visit includes:
- Patient and provider locations
- Mode of communication (e.g., video, phone)
- Patient consent
- Start/end times
- Clinical notes justifying medical necessity
Be Ready for Audits
Medicaid may audit telehealth claims months or years later. Expect requests for:
- Full documentation
- Proper coding (CPT, modifiers, POS)
- Proof of HIPAA-compliant tech use
How Health Quest Can Help with Medicaid Telehealth Billing
At Health Quest, we simplify Medicaid telehealth billing so you don’t have to worry about coding errors, state-specific rules, or enrollment hurdles. Our team handles everything from policy reviews to multi-state billing support and CAQH/PECOS/EDI setup. If you’re offering telehealth, we’ll make sure you get paid for it accurately and on time.
Final Thought:
Telehealth is no longer an emerging option; it’s a core part of how Medicaid patients access care. As reimbursement policies evolve, providers have a unique opportunity to expand access, reduce missed visits, and grow revenue streams. However, success depends on staying current with state-specific rules, billing accurately, and documenting every detail. At Health Quest, we’re here to help you deal with Medicaid telehealth billing with confidence, compliance, and clarity so you can focus on patient care, not paperwork.