Medicare billing as a healthcare provider can be complex, but if you want to get reimbursed it is essential that you bill Medicare accurately. Medicare’s improper payment rate was 7.66%, totaling $31.7 billion, with the majority of errors stemming from missing documentation, incorrect coding, and medically unnecessary services. To avoid these issues, providers must see if the documentation is accurate, follow proper coding guidelines, and stay updated on medicare regulations to minimize claims denials and ensure timely payments.
In this guide, we’ll walk you through the essential steps and tips for getting paid efficiently while maintaining compliance with Medicare’s guidelines.
What is Medicare?
Medicare is a federal health insurance program for people aged 65 and older, and for some younger individuals with disabilities or specific medical conditions. It covers hospital stays (Part A), outpatient services (Part B), prescription drugs (Part D), and additional services through Medicare Advantage (Part C). While Medicare helps reduce healthcare costs, it doesn’t cover all expenses, so beneficiaries may still need to pay premiums, deductibles, and co-payments.
Here’s a table summarizing the four main parts of Medicare:
| Medicare Part | Description |
| Part A | Hospital Insurance (covers hospital stays) |
| Part B | Medical Insurance (covers outpatient services) |
| Part C | Medicare Advantage (a private plan that includes A, B, and often D) |
| Part D | Prescription Drug Coverage (covers medication costs) |
Who is a Medicare provider?
A Medicare provider is any individual or organization that delivers healthcare services to Medicare beneficiaries and is approved by Medicare to bill for those services. Providers can include:
- Doctors (e.g., primary care physicians, specialists)
- Hospitals (e.g., inpatient, outpatient facilities)
- Clinics (e.g., urgent care, mental health centers)
- Nursing facilities (e.g., skilled nursing homes)
- Pharmacies (for prescription drug services)
- Home health agencies (providing care at home)
Getting approved as a provider requires proper Medicare credentialing service, followed by maintaining compliance through accurate Medicare billing.
How to Bill Medicare as a Provider
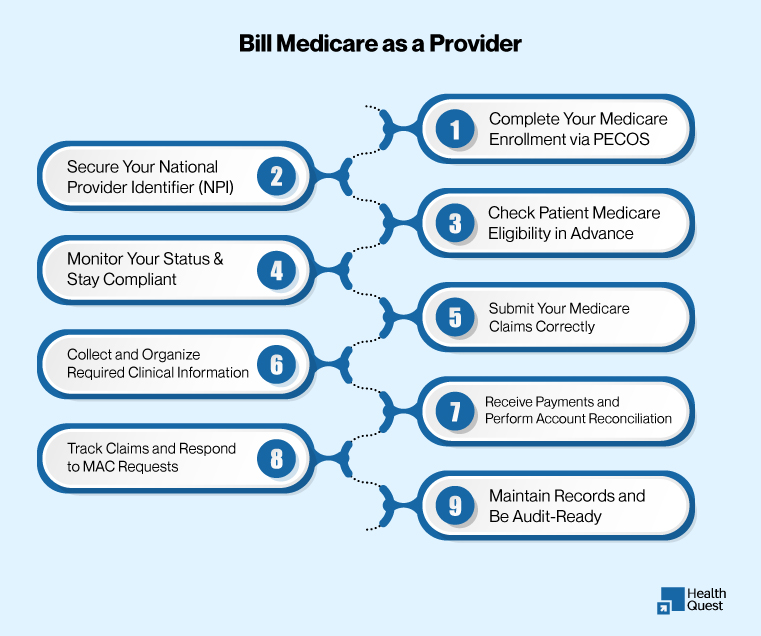
Billing Medicare requires a step-by-step process, from enrollment to payment reconciliation, ensuring compliance and maximizing reimbursement.
Secure Your National Provider Identifier (NPI)
The first step to enrolling as a Medicare provider is obtaining a National Provider Identifier (NPI), a unique 10-digit number required for billing, verifying credentials, and communication with payers. Apply for your NPI through the NPPES Portal by providing personal and business details, including licensing information.
Complete Your Medicare Enrollment via PECOS
After securing your NPI, the next step is enrolling with Medicare. Use the PECOS (Provider Enrollment, Chain, and Ownership System) to submit your application. Depending on your role, you’ll complete the CMS-855I form for individual providers or the CMS-855A form for facilities. Attach all necessary documentation and confirm your details before submitting.
Monitor Your Status & Stay Compliant
Enrollment doesn’t stop at submission. You must actively monitor your status with Medicare, especially revalidation notices that occur every 3–5 years. Update your information in PECOS if there are any changes to your address, tax ID, ownership, or licensure. Keeping up with the latest Medicare billing rules is also crucial for maintaining compliance.
Check Patient Medicare Eligibility in Advance
Before providing services, always verify your patient’s Medicare eligibility. This can be done using your Electronic Health Record (EHR) system, the Medicare Eligibility Inquiry Tool, or through your local Medicare Administrative Contractor (MAC). Regular eligibility checks help prevent service complications or claim denials due to coverage changes.
Collect and Organize Required Clinical Information
Ensure all documentation is accurate and secure before billing Medicare. Gather all necessary details, including correct CPT/HCPCS and ICD-10 codes, signed patient consent forms, treatment orders, progress notes, and medical necessity documentation. Proper documentation is key to avoiding claim rejections or denials.
Submit Your Medicare Claims Correctly
Once the services are provided and documented, it’s time to submit your claims. Medicare accepts two types of claim submissions:
- Electronically through Medicare’s EDI system (preferred and fastest)
- Paper Claims via the CMS-1500 form (if exempt from EDI)
Track Claims and Respond to MAC Requests
After submitting claims, stay on top of any follow-up actions from your local Medicare Administrative Contractor (MAC), such as rejections, additional documentation requests (ADRs), or payment adjustments. Respond quickly to avoid delays in payment or further complications.
Receive Payments and Perform Account Reconciliation
Once approved, Medicare payments are transferred electronically (EFT) into your designated bank account. Review the Medicare Remittance Advice (RA) to understand any deductions or adjustments. Ensure you follow up on unpaid or underpaid claims promptly.
Maintain Records and Be Audit-Ready
Medicare requires providers to keep comprehensive records for at least 10 years. This includes patient encounter notes, lab results, signed consents, and billing data. Use secure, HIPAA-compliant Electronic Health Records (EHR) systems and regularly back up your data. Be prepared for unannounced audits or medical reviews at any time.
Common Billing Errors and How to Fix Them
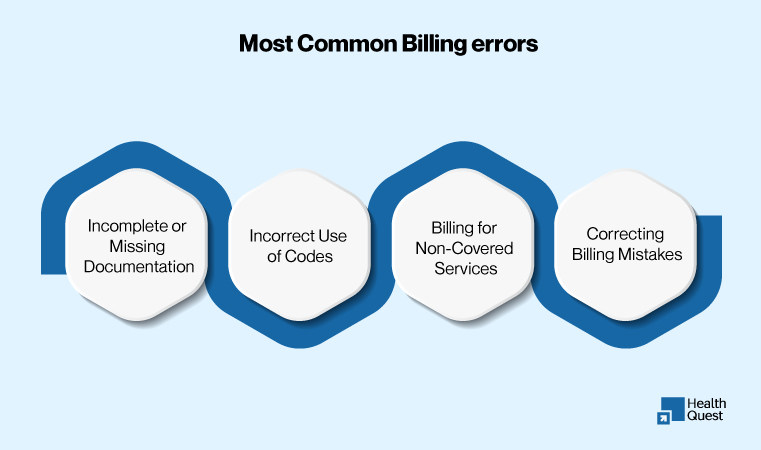
Billing errors can cause denials, delays, and reduced reimbursements. Here are common mistakes and how to prevent them:
Incomplete or Missing Documentation
Missing documentation is a leading cause of claim denials. Always ensure you include all required records, such as patient consent and treatment orders. Use EHR systems to stay organized.
Incorrect Use of Codes
Using incorrect ICD-10 and CPT codes can lead to payment delays. Keep your coding knowledge updated and use tools to minimize mistakes.
Billing for Non-Covered Services
Billing for services not covered by Medicare can result in denials. Always check Medicare’s coverage guidelines before submitting claims to avoid errors.
Correcting Billing Mistakes
If a claim is denied or rejected, resubmit it with the correct documentation or updated codes. Follow the appeal process to resolve issues and prevent further delays.
Medicare Reimbursement Process
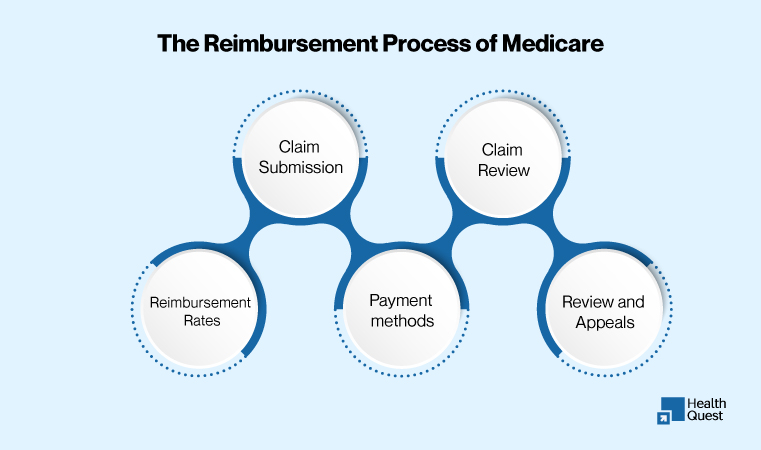
The Medicare reimbursement process ensures providers are compensated for services rendered to Medicare beneficiaries. Understanding how claims are processed, the role of the Medicare Physician Fee Schedule, and payment methods is essential for timely and accurate reimbursement.
How Payments Are Processed
Medicare processes claims through a structured process, evaluating the medical necessity of services under its Fee-for-Service system. After submission, Medicare reviews the claim, and if approved, the provider is reimbursed according to set rates. Claims may be denied if they don’t meet the required criteria, so providers need to ensure they are following all guidelines to avoid delays.
Here’s how it works:
- Claim Submission: Providers submit claims (electronically or on paper) following Medicare guidelines.
- Claim Review: Medicare reviews the claim for accuracy and medical necessity.
- Reimbursement Rates: Payments are based on the Physician Fee Schedule (MPFS).
- Payment Methods: Providers are paid via Electronic Funds Transfer (EFT) or paper checks.
- Review and Appeals: If a claim is denied, providers can correct and resubmit or appeal.
Understanding Medicare’s Fee Schedule
The Medicare Physician Fee Schedule (MPFS) is a key tool for determining reimbursement rates for services. It assigns a specific dollar amount to each procedure based on factors like complexity and region. Providers should familiarize themselves with the MPFS to understand what they will be paid for various services and ensure they’re within compliance.
Receiving Payment
Once claims are approved, providers can receive payment in different ways:
- Electronic Funds Transfer (EFT): Payments are directly deposited into the provider’s bank account, making it the quickest and safest method.
- Paper Checks: In some cases, Medicare may issue payments via checks, though this is becoming less common.
Best practices to ensure accurate billing:
There are several tips you can follow to ensure that the billing is done correctly.
Stay Current with Medicare Policies
Regularly update your knowledge of Medicare regulations and billing codes. Medicare rules change frequently, and staying informed ensures your claims are compliant and minimizes errors.
Use Billing Software
Utilize billing software to improve your processes, reduce human error, and ensure proper documentation. Automation helps save time and improve accuracy in claim submissions.
Work with a Medicare Billing Specialist
Consulting a Medicare billing specialist can ensure your billing practices are accurate and compliant with all regulations. Their expertise can help prevent costly mistakes and claim denials.
Final Thought:
Accurate Medicare billing is the foundation of timely reimbursement, while proper Medicare credentialing services ensure providers are eligible to receive payments in the first place. By staying updated on regulations, using billing software, and consulting Medicare billing specialists, providers can minimize errors, reduce denials, and improve revenue flow.