Are you constantly getting stuck on the insurance eligibility verification process? Don’t worry, a lot of healthcare providers do. This blog covers exactly why you need to conduct this process.
We will also explain how you can effectively conduct it to deliver positive results. Read on to find out how you can successfully verify the insurance coverage of your patients.
In addition, maximize coverage with our insurance eligibility verification services. Boost efficiency & accuracy for your insurance processes. Get a free consultation!
What Is Insurance Eligibility in Medical Billing?
Insurance eligibility in medical billing is a process in which healthcare organizations inspect their patients’ insurance coverage. With insurance eligibility, you can settle the eligibility of your patients to reimburse payments for the medical services provided to them.
Therefore, it is an important process for medical billing as it provides valuable insights into the payment of medical bills. Verification of patient insurance information like pre-authorization requirements and benefits is crucial for effective medical billing.
How Insurance Eligibility Works in Medical Billing?
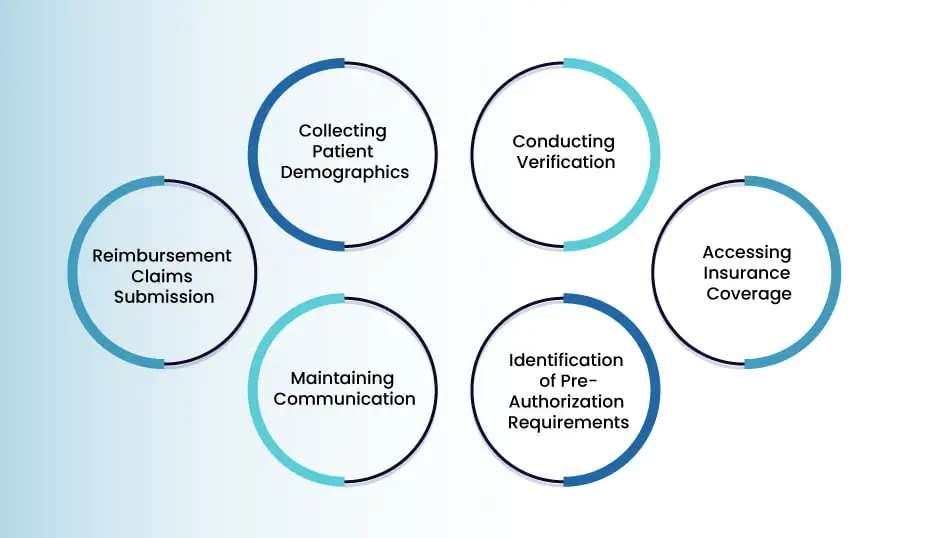
There are various processes involved in verifying the insurance eligibility of patients to generate accurate medical bills. They largely comprise the collection of demographic entries, initiation of verification, and accessing insurance coverage information. Let’s look at these processes and many more, along with how they can navigate your medical billing:
1. Collecting Patient Demographics
The process of medical insurance eligibility verification is initiated with the collection of patient demographics, primarily insurance coverage. You can record details about their insurance providers and the healthcare services covered by them.
With this, you can estimate the eligibility of your patients to avail of your medical treatments. Accurate medical bills can be generated with the agreement of all relevant parties to ensure a smooth process.
2. Conducting Verification
You must also verify the details provided by your patients. Verification can be conducted through either an insurance eligibility verification software or by your billing staff. Either way, you must contact the insurance providers of your patients. In this way, you can maintain a standardized verification system for their information.
3. Accessing Insurance Coverage
Information about the insurance coverage of your patients is also crucial for your medical billing operation. You must access it as well so that you are aware of their insurance coverage. With it, you can utilize their coverage limits, deductibles, and copayment amounts to determine their eligibility in medical billing as well.
In addition, you can also derive specific restrictions or exclusions for the generated medical bills. They may apply to your patients based on their insurance coverage.
4. Identification of Pre-Authorization Requirements
Pre-authorization requirements refer to the agreements by insurance companies to reimburse payments for specific healthcare services. You must identify them beforehand for all your medical treatments and procedures through your patients and their insurance providers.
You can direct your patients to hand in every pre-authorization requirement to you. They must also ensure that their insurance providers have given approval for the relevant procedures.
5. Maintaining Communication
You must be in constant communication with your patients during the verification of their insurance eligibility. It is vital to ensure that their medical bills are appropriately generated. Insurance coverage details can be shared with them so that they are kept in the loop throughout the procedure.
You can inform them about their deductibles and copayments, along with any additional expenses. This will prevent any unnecessary denials from them, as they will already be in sync.
6. Reimbursement Claims Submission
The final process of verifying the insurance eligibility of patients is the submission of reimbursement claims. They have to be submitted to them and their insurance providers. You have to include important documentation like procedure codes and medical records.
They should detail all the healthcare services availed and their relevant medical bills. In this way, you must follow the standardized procedure to submit accurate reimbursement claims. As a response, insurance companies reimburse payments accordingly.
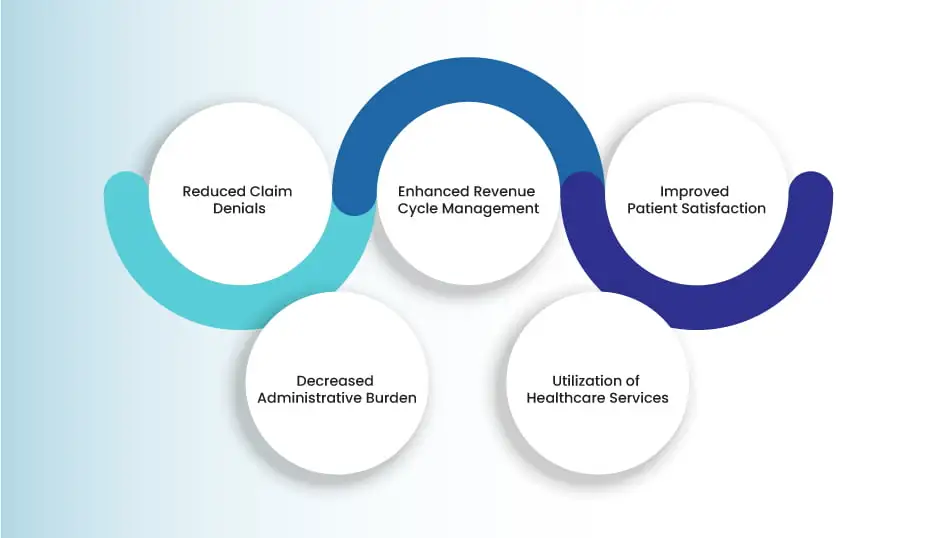
Importance of Insurance Eligibility in Medical Billing
Insurance eligibility holds immense importance for you in medical billing. An accurate medical insurance verification process of your patients’ eligibility can reduce claim denials from their insurance providers.
You can also enhance your revenue cycle management and improve patient satisfaction. All of these factors significantly decrease your administrative burden and enable you to appropriately utilize your healthcare services.
1. Reduced Claim Denials
Accurate verification of insurance eligibility ensures that accurate information about patients is provided to their insurance providers. In this way, the chances of detecting irregularities in the insurance coverage of your patients are reduced.
Therefore, insurance companies are also less likely to submit denial claims for your healthcare services. By doing this, you also save yourself from encountering financial losses or unpaid bills as a result of rigorous background checks.
You are in control of the insurance eligibility process from the start and can identify any issues instantly. It enables you to streamline medical billing by accurately billing your patients based on their eligibility and preventing reimbursement rejections.
2. Enhanced Revenue Cycle Management
You can enhance your revenue cycle management as well by checking the insurance eligibility of your patients. By determining the status of their financial responsibility, you can get ahead of any outstanding balances and deductibles.
With this, you can appropriately collect payments from them at appropriate times for your services. Your cash flow will steadily rise with a subsequent impact on your accounts receivable.
Moreover, you will experience a smooth revenue cycle with an increase in profits and a decline in expenditure, which will stabilize your financial situation. In this way, you can focus better on providing quality care to your patients.
3. Improved Patient Satisfaction
Patient satisfaction is vital for standardized medical billing in healthcare organizations. Patients are largely satisfied with transparency in their relationship with insurance companies and healthcare providers. You can tip into this factor by accurately regulating healthcare costs.
Financial burdens on patients can also be prevented by maintaining a sufficient record of details about their insurance coverage. You can also establish up-to-date communication with them and provide unambiguous guidelines about any additional expenses or insurance plans.
As a result, your patients will feel well-informed to make knowledgeable decisions about their medical procedures and treatments. This builds a positive perception and trust for your healthcare organization, and they are more likely to come again in the future.
4. Decreased Administrative Burden
By effectively conducting these processes, you are less likely to experience administrative burdens. You can save precious time and resources as a result of a proper insurance eligibility verification process.
In addition, fewer appeals and claim denials also decrease complexities for your administrative staff. In this way, they can work efficiently to generate the medical bills of your patients, which will optimize the medical billing process.
You will be able to conduct an effective allocation of your resources and focus on your administrative operations. This will progress your healthcare organization to an ideal position to manage your patients.
5. Utilization of Healthcare Services
You can also appropriately utilize your healthcare services by accurately verifying the insurance eligibility of your patients. Patients can make better decisions to timely seek healthcare services when they are in the loop about their financial situation and insurance coverage.
This creates a proactive approach with which you can curate ideal health outcomes for your patients. It will be based on the appropriate need of your healthcare services. Keep in mind that any irregularities in insurance coverage can delay medical treatments.
Therefore, you must ensure an accurate insurance verification and eligibility of pre-authorization requirements as well. It will decrease any unwarranted delays and ensure specialized access to your healthcare services to patients.
What Are The Methods Of Verifying Insurance Eligibility?
There are two main methods of accurate verification of patient eligibility:
1. Electronic Checks
Electronically verifying the insurance eligibility of patients is the most efficient method. It can instantly check if they are eligible to receive your services. There are a lot of online resources available that can help you.
2. Manual Checks
This method is less efficient than electronic checking. However, it is an ideal option if you cannot access electronic eligibility checks. You can conduct a manual verification by calling the relevant insurance company. You can also ask them to provide their insurance card.
Benefits of Insurance Eligibility Verification
Health insurance eligibility verification can benefit both patients and healthcare providers. Here’s how:
1. How Does Insurance Eligibility Verification Benefit Providers?
Healthcare providers can conduct this process to find out what their patients owe for their services. It helps you collect those payments at the time of medical procedures and treatments. You can also get authorizations from the insurance companies for those services.
Hospitals can get clean claim rates as they are able to bill the correct insurance. They can also determine the billing order if their patients have multiple active policies.
2. How Does Insurance Eligibility Verification Benefit the Patient?
Verifying the insurance coverage of patients helps them plan for their financial responsibility. This way, they do not have to take stress or worry over their medical bills. It also enables them to look for a lower-cost hospital or some other insurance policy.
Tips for Verifying Insurance Eligibility
You can ensure the completion of effective insurance eligibility verification services by following these tips:
1. Insurance Verification Checklist
You should ask the right questions while you are verifying the insurance coverage. Your staff should enter details from the insurance card of your patients. They can also call the relevant insurance company or use electronic eligibility systems. The information needed for the medical records includes the insurance name.
The phone number and claims address are also required along with insurance ID. Keep in mind that the insured is not always the patient. So you need their relationship to the patient as well. These are just some of the many details required.
2. Copy of Insurance Card
You must also ask for a copy of the insurance card of your patient. It is still a good idea even if the card is the same as before. The copy should contain updated images of both sides of their insurance card. Your electronic health record should have a backup in case a patient mistyped their information. The ID numbers should also be double-checked before the claims are sent.
3. Contact the Insurance Provider
Insurance coverage can even change or stop just after some weeks. So, you must contact the insurer to recheck the medical billing eligibility. Hospitals usually place a phone call or use their billing system. The system is used for larger insurers like Medicaid, Medicare, or Blue Cross.
This is the most efficient option if you have an electronic eligibility system. Sometimes, you can even import data directly into your record systems. It makes the process faster and avoids data-entry errors.
4. Record Accurate Information
Your staff should be trained enough to accurately record patient information. Those details are important for your medical claims. Even a small mistake can turn a clean claim into a denial. Rushed verification practices and data mistakes can lead to delayed payments. The reimbursement claim can also go unpaid.
5. Patient Follow Up
You must always follow up with your patients in case of any questions or concerns. Hospitals set up a portal to inform their patients. They either do that through email or over the phone. You can let your patients know about any copays or other issues. You are more likely to get your funds if you quickly inform them about any out-of-pocket expenses.
What Are The Benefits Of A Standard Operating Procedure (SOP) For Checking Patient Eligibility?
Hospitals should also create an SOP for their eligibility workflow. You can include a recommended talk track for your staff. It will help them request balances of patients. You can also document the ideal processes for your practice.
The SOP document can also enable your staff employees to collaborate with each other. They can understand the impact of their practices on the revenue cycle.
Benefits Of Outsourcing Insurance Eligibility Verification
Outsourcing the insurance eligibility verification process can bring a lot of benefits for hospitals. Let’s take a look at the top 3 benefits:
1. Cost-Effectiveness
An in-house billing team managing insurance-related tasks can have huge financial costs. You have to recruit, train, and then retain that staff. Apart from that, top-level technology and software are also needed. All this can accumulate a lot of costs.
Outsourcing does not involve any of these overhead expenses. Top outsourcing companies have flexible pricing models. They are cost-effective and use your resources efficiently.
2. Expertise
You can also get access to the expert billing professionals of outsourcing companies. They have in-depth medical coding knowledge as well. They are able to effectively handle the insurance policies and procedures. With their expertise and knowledge, you can ensure an efficient submission of accurate claims.
3. Enhanced Efficiency
By outsourcing your billing, you have more time and resources to manage other processes. Instead of going back and forth with their responsibilities, your staff can focus on the main tasks. They include patient care and increasing revenue. On the other hand, the outsourcing company can manage your revenue cycle management process.
They will reduce your administrative burdens and increase the overall efficiency. This way, you have a faster and smoother revenue cycle. Your cash flow increases at a smooth rate due to fewer claim denials.
The Bottom Line
Healthcare organizations rely on insurance eligibility to ensure streamlined financial workflows. You must also not neglect its importance for the seamless functioning of your medical services. We at Health Quest Billing are equipped with modern healthcare resources and top-notch expertise to manage your medical operations. Contact us today and skyrocket your revenue with 4x faster collection.







 12 mint read
12 mint read