Did you know a perfectly executed payment posting can ensure 4x faster collection for your healthcare? It fills the gap between your medical services and financial processes. This blog will fully explain the multifaceted process of payment posting.
We will dissect its steps and learn how to do payment posting in medical billing. You can also find details about the benefits and methods of payment posting. Continue reading further to know how this process can streamline your medical billing.
Additionally, optimize your medical billing with our payment posting services. Get accurate, timely reimbursements. Enhance your revenue cycle management now!
What Is Payment Posting in Medical Billing?
Payment posting in medical billing is a process in which you can record and reconcile the payments you receive from patients and insurers. It is also called cash posting in medical billing. This process involves accurate documentation of paid bills and tracking of outstanding balances.
You also have to maintain financial accuracy in payment posting by matching received payments to billed services. This approach minimizes discrepancies and streamlines revenue management to enhance your billing cycle.
Steps Involved in Payment Posting
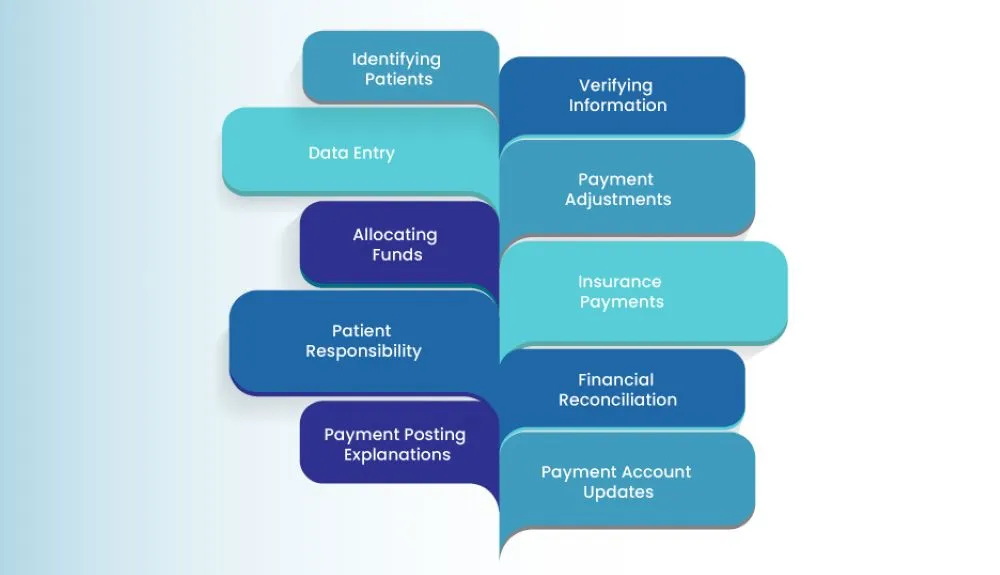
1. Identifying Patients
This step is the first one in payment posting for medical billing, in which the received payments are matched with their corresponding invoices and patient accounts. This strategy ensures an accurate attribution of those payments with the appropriate medical services availed.
You can prevent errors and confusion by reviewing and cross-referencing the payment documents. The information provided mostly includes demographic entries, invoice numbers, and service descriptions. It confirms the authenticity and correctness of the received payments.
In addition, you can flag any discrepancies or mismatches for further investigation and then move forward with the rest of the payment posting process. This way, you can track the relevant income sources, monitor payment trends, and address any potential irregularities.
2. Verifying Information
The payment information also has to be verified in the payment posting process in medical billing. Such information usually includes payment amount, method, and payer information. It is thoroughly reviewed in this step to confirm its authenticity and correctness.
You have to comprehensively compare the provided payment details with the information mentioned on the associated invoice and patient records. With this scrutiny, you can identify any errors that could cause incorrect account updates or financial imbalances.
This validation contributes to a reliable payment posting in the revenue cycle management process. With such validation, you can properly allocate funds and maintain your integrity. This step is crucial as inaccuracies can have ripple effects on financial processes.
3. Data Entry
After verifying those details, you can also enter them into your billing system to maintain accurate record-keeping. This action creates a digital trail of the transaction in which details such as payment date and amount are recorded into the medical billing software.
This electronic documentation serves as your reference for future audits, reconciliation, and patient billing inquiries. Furthermore, you can also minimize the risk of errors and ensure a seamless transition from payment receipt to account updates.
An organized record of financial transactions enhances the efficiency of your payment processing. In this way, you can maintain an accurate financial ledger and enable a reliable audit trail for compliance and accountability.
4. Payment Adjustments
Payment adjustments are a pivotal step in which healthcare organizations address discounts and contractual agreements. You can apply any contractual adjustments or discounts applicable for the services availed to the payments received.
For this step, you have to review your terms of agreements with insurance companies to ensure accurate adjustments. In addition, you can apply pre-negotiated discounts or write-offs with which those payments are aligned with the agreed-upon rates.
By properly applying adjustments, you can maintain transparency in your billing and financial transactions. Precise adjustments contribute to your financial accuracy and accountability and prevent overbilling and underbilling. These measures foster trust with patients and insurers.
5. Allocating Funds
In this step, funds received in the form of payments are divided among various billed services or charges based on the invoice details. You have to extensively review the associated invoices and identify the individual services or treatments availed by your patients.
You have to assign portions of those payments to your specific services to reflect the actual charges incurred. By granularly allocating portions, you can maintain financial accuracy and clearly break down the sources to which those payments are applied.
By executing this step, you can correctly distribute the received payments and prevent confusion and disputes. Furthermore, you can also track the financial performance of your medical treatments, understand revenue patterns and make informed pricing decisions.
6. Insurance Payments
Insurance payments can be executed by healthcare organizations, but keep in mind that they are particularly for insured patients. This step involves the allocation of the payments received from insurance companies to their respective patient accounts and services availed.
Initially, you have to verify the payment details against your insurance claims and then allocate those payments to their corresponding medical services. You must appropriately address both primary and secondary insurance companies, if applicable.
In this way, you can reduce outstanding balances and streamline your revenue cycle, as insurance payments can be accurately processed. Moreover, you can also maintain positive relationships with insurers and accurately bill your patients for their availed services.
7. Patient Responsibility
You can also accurately record payment details that are your patient’s responsibility, such as deductibles or copays. To record them, you have to review the patient’s insurance policy and billing details to determine the amount that they are obligated to pay.
You must ensure that this patient responsibility portion is accurately noted and reflected in the payment posting records. This step maintains transparency with your patients in terms of their financial obligations for the medical services availed.
It also establishes financial clarity and trust between you and your patients. Your patients become aware of their financial obligations and the appropriate balances of their accounts. In addition, you can enhance communication and reduce medical billing disputes.
8. Financial Reconciliation
Financial reconciliation is another vital step in which received payments are cross-referenced with the bank deposits as well. It certifies higher accuracy as those payment records in the billing system are compared with the actual deposits made into your bank accounts.
This step enables you to promptly address any inconsistencies to prevent financial drawbacks. Furthermore, you can contribute to the financial integrity of your medical billing process with the identification and rectification of the errors existing in your payment posting in RCM.
In this way, your financial records align with actual bank transactions and reduce the risk of financial mismanagement. Furthermore, you can also identify any missing transactions that may require further investigation.
9. Payment Posting Explanations
You can aid your communication with patients by adding relevant comments or explanations to the payment records. To do this, you can include notes to provide additional context for specific payment details, adjustments, and exceptional circumstances.
These notes can be later used as references and can be helpful in future inquiries, audits, and billing-related discussions. They also facilitate transparency and accuracy in your financial records by documenting pertinent information.
You can effectively communicate with other departments in your healthcare organization. Furthermore, you can also offer insights into the reasons behind the clarifications for payment discrepancies. Internal coordination can be enhanced to reduce confusion for your patients.
10. Payment Account Updates
Your patients’ accounts can also be regularly adjusted so that you can accurately manage your accounts receivable. You must review the payment allocation, adjustments, and relevant notes before those accounts are updated.
By doing this, you can ensure that the account balance is correctly adjusted and the financial status of your patients is accurately represented. Accurate account updates also lead to transparent financial records and optimized patient communication.
You can also seamlessly report and analyze your financial standing. It is possible by maintaining precise records of the payments received and the services availed. Moreover, you can also maximize accountability by conducting rigorous audits and compliance checks.
Why Is Accurate Payment Posting Important?
Many doctors consider payment posting as the most important process in medical billing. It enables them to track their incoming payments. Payment posting identifies and solves most of the billing challenges. It covers each patient’s payment along with regular insurance costs and checks.
Any mistake in payment posting medical billing can affect the accuracy of claims submission. A hospital may incorrectly post its insurance payment. In this case, secondary and tertiary payers are more likely to receive that incorrect bill.
Benefits of Payment Posting in Medical Billing
Since payment posting is a highly important process, it has a lot of benefits for hospitals. Let’s look at the major ones below:
1. Revenue Cycle Analysis
First, payments have to be posted to the relevant patient accounts. Then, you have to analyze the revenue cycle of your medical office. This way, you can identify opportunities where you can increase your cash flow. An effective analysis increases profitability, which leads to a better revenue cycle. It can also improve the accounts receivable departments of hospitals.
2. Repetitive Problems Solved
There can be several repetitive problems with a revenue cycle at the same time. And you can only solve them with effective payment posting. In this process, you have to conduct medical payment posting along with any claim denials and adjustments. You must identify the denials first to resolve them. This practice prevents future claims denials for the same reason.
3. Improves Billing Processes
Payment posting also determines the efficiency of your billing staff. In some cases, their revenue cycle may be unable to function optimally due to their processes. As a result, you may have to first identify the problem. This way, you can determine whether you have to add, remove, or improve a billing process. These changes will make your revenue cycle effective.
Steps in Ensuring Accurate Payment Posting
There are certain steps that you can take to ensure that you conduct accurate medical billing payment posting. We have covered those steps in detail for you:
1. Adjudication
In adjudication, insurance companies review the claims submitted by hospitals. They use that review to determine the reimbursement amount. It is determined based on the insurance coverage of their patients. Insurance companies also use their contracts with hospitals.
As an added measure, some companies use the medical codes assigned as well. They also send either Remittance Advice or an Explanation of Benefits to hospitals. With these documents, insurers inform hospitals about the amounts they will pay as reimbursements.
2. Reconciliation
Payment reconciliation is an important step while posting payments for medical billing. It compares and verifies the payments received from insurers. There are other payments incoming from government programs as well.
They are according to the billed charges of your medical services. You can also ensure that the payments collected are credited to your bank accounts. You just have to compare the Electronic Remittance Advices with the relevant bank deposits.
3. Balancing and Reporting
Hospitals have to balance their accounts after resolving their discrepancies. Then, they can generate reports to monitor their payment trends. Those reports also help them identify areas for improvement. This way, hospitals can maintain accurate financial records through payment posting.
How To Evaluate The Payment Posting Process
Hospitals must evaluate their payment posting process to utilize its full potential. Here is how you can evaluate yours for optimum results:
1. Define Key Metrics
You can try defining the key metrics for the quality and efficiency of your processes. Some major metrics include the turnaround time, accuracy, and discrepancy of payment posting. Hospitals can define those metrics through their historical data and organizational targets. This way, they can compare their performance against them.
2. Automate Billing Workflow
With an automated workflow, you can measure the value of your payment posting. It can also reduce your manual work along with any delays and errors. You can use the relevant tools and technology for automation. This way, you do not have to use statements and paper checks for scanning and data entry.
3. Communication and Collaboration
Communication is always important in medical billing. It gives you a chance to collaborate with your stakeholders. They can include patients, insurance companies, and your billing staff. You can use your automated billing workflow and metrics to inform them about payment posting best practices. This way, you can get their feedback on your processes and responsibilities. This practice is an effective way to coordinate your activities with your stakeholders.
What are the Methods of Payment Posting
There are two methods of payment posting. They are named manual and auto posting. Find out more details about them below:
Your administrative staff has to fill out manual posting. This is why this method takes more time. As a result, many problems can arise and delay manual posting. One of the major problems in this method is typos. Such problems are more likely to occur in medical billing.
Auto payment posting is completely different from manual posting. It makes your billing process faster instead of delaying it. It is a software-driven strategy that is more reliable in terms of revenue collection. You can use this method to gain better control over your medical billing. Auto posting is especially important for your day-to-day matters.
What Does a Medical Payment Poster Do?
A medical payment poster has to manage the payment posting processes for their hospital. This management can be either electronic or manual. They have to maintain billing records and revenue documents.
These documents are mostly about patient payments and insurance reimbursements. Payment posters may also have to transfer any deductible balances. Hospitals also need them to review the balances of their patient accounts.
This helps those hospitals to determine their posting accuracy. They may also be required to perform reconciliations for their bank and hospital payments. As an added role, payment posters can also study and resolve any unapplied medical accounts.
Furthermore, optimize revenue with efficient charge entry in medical billing. Discover expert tips & tools. Streamline your billing process today!
How Health Quest Payment Posting Services Can Improve Your Healthcare Practices?
Health Quest Billing has expert medical billers who can analyze your underpayments. They can identify and solve your payment discrepancies. This way, you can determine why some of your payments received are less than the amount you billed. As a result, you can take relevant measures to get accurate revenue for your services.
We can also help you with payer trend analysis. Health Quest Billing can examine your payer behaviors and patterns. That data can be used to increase your cash flow. You can also make strategies to overcome your billing complexities.
Moreover, healthcare organizations face numerous challenges of payment posting. Find out how outsourcing payment posting services can reduce errors and increase efficiency.
The Bottom Line
The payment posting process has a lot of aspects that hospitals must be mindful of. You should manage them effectively to maintain financial accuracy and transparency. There are certain steps that you can take to maintain accurate payment posting.
We also discussed how you can evaluate it to avail its benefits. You must also know the differences between its methods to know which one suits you. Contact Health Quest Billing to learn how your payment posting can upscale your revenue.







 13 mint read
13 mint read
